Register for prenatal sessions
Mount Lebanon Hospital
+961 5 957 000 – 15271
Mount Lebanon Hospital’s highly trained obstetricians, maternal fetal medicine specialists, and certified midwives prepared this booklet for all expecting mothers, to help them prepare themselves, their spouse and family for the baby’s arrival.
We offer delivery rooms, Neonatal Intensive Care Unit – NICU and Blood bank. Our Obstetrics and Gynecology department is offering Prenatal and Postnatal Education sessions. These classes are given by a highly trained team of midwives and physical therapists, benefits include:
What can be more beautiful than bringing a new life into the world? Happy Midwives Day to the caring hand that accompanies women along their journey to motherhood

Motherhood is a choice you make everyday. Choose MLH for a journey well started
- Help build your confidence in your body’s ability to give birth;
- Calm your fears and prepare you for birth;
- Opportunity to openly discuss curiosities and concerns;
- Knowledge of options and choices available;
- Your partner will learn about childbirth and how to support you on the big day;
- Information about:
- Nutrition and exercise importance,
- Healthy lifestyle,
- Labor: Step by step medical procedures,
- Pain management breathing and relaxation techniques,
- Breastfeeding,
- Postpartum care: mother & baby.
We are excited to be a part of your birthing and family healthcare team and hope you will continue to rely on us for all your healthcare needs

What can be more beautiful than bringing a new life into the world? Happy Midwives Day to the caring hand that accompanies women along their journey to motherhood.


Additional references:
Part 1: Guide for expecting mothers
What to expect during pregnancy
A. Body changes


Many transformations occur during the Nine Months of pregnancy.
It is important to know that all changes will return to normal 2 months to 1 year after giving birth.

Symptoms and early signs of pregnancy include:
the absence of menstrual periods changes in the breasts, fatigue, nausea, and mood swings.
i. Mouth and oral health
Bleeding Gums and swollen gums are common pregnancy complaints, caused by the increase in your circulation volume and certain hormone supply and may lead to an infection. It is very important to take good care of your oral hygiene to prevent gingivitis or gum inflammation. To insure healthy teeth and gums:
- Brush and floss regularly
- Get a dental checkup early in your pregnancy
- If you experience any problems consult your dentist
ii. Skin

The Pregnancy Line, which is more officially called Linea Nigra, is the dark line that develops across the belly during pregnancy. It is possible that the line may have previously been there, however because it was so light in color it went unnoticed. According to the American Academy of Dermatology, 70% of women develop Linea Nigra during pregnancy. While the specific causes of the Linea Nigra are unknown, one theory is that melanocyte-stimulating hormone created by the placenta is the main contributing factor. This hormone is also believed to cause the darkening around the nipples. The good news is that it usually lessens and fades away shortly after birth.
Stretch marks: Pinkish lines, forms when the normal skin is not elastic enough for stretching required during pregnancy, typically seen on a woman’s abdomen, breasts, backside or thighs and they tend to itch. They most likely occur among women who are obese. While they won’t disappear completely, stretch marks will fade after delivery and are usually preventable. It is recommended to use a cream to help relieve stretch marks and itchiness (prescribed by the physician).
Pregnancy Mask: Due to an increase in Melanin hormone, brownish patches of dark skin, may appear on the face around the eyes, over the cheeks and nose.
Linea nigra: Fluctuating hormone levels can produce a dark line in the middle of the abdomen running from the belly button down to the pubic bone, usually common among women with a dark complexion.
iii. Hair
Estrogen increases hair growth, therefore extra hair grows not only on your head, but on your body also, such as the upper lip, stomach, back and around the areolas.
iv. Nails
During pregnancy your nails’ texture coarsen, therefore they become brittle and soft. That’s a result of an increased blood flow to the fingers and toes due to an increased estrogen level.
v. Breast
Pregnant woman’s breasts become full and tender, they may increase in size as milk glands enlarge and fatty tissue increases. The nipples become more sensitive to the touch, and the areolas surrounding the nipples will darken and enlarge and bluish veins might also appear. During the third trimester, the nipples may start leaking colostrum (milk fluid). We recommend to:
- Wear a supportive bra.
- Choose cotton bras
- Increase your bra’s size as your breasts become larger, it should fit well without irritating your nipples. Try maternity or nursing bras, which provide more support and can be used after pregnancy.
- Tuck your choice of nursing pads into each bra cup to absorb leaking fluid.
- Clean your breasts with warm water only. Do not use soap or other products.
- Use moisturizing nipple cream, twice a day, starting from the seventh month of pregnancy.
vi. Joints and ligaments
Relaxing, a pregnancy hormone, relaxes the pelvis ligaments preparing for labor and delivery, as it stretches joints and ligaments all over the body. It can lead to back pain and sciatica. In the lower back and runs through the backside and downwards to the leg. Relaxin is responsible for the “pregnancy waddle”, an altered walk resulting from a bigger baby bump and an increased spine curvature.
vii. Body temperature
Women will tend to feel warmer and sweat a lot during pregnancy due to an increased metabolic rate and sweat gland activity.
You should wear loose clothing, stay chilled, and drink a great amount of water every day.
viii. Feet and legs
Swelling in the feet and ankles (edema): May occur because of hormonal changes as your body is producing extra fluids and your uterus is growing, which pressures your veins.
Varicose veins: Can appear in the legs, vagina and rectum (hemorrhoids) and are usually hereditary.
Leg cramps: Pressure from the growing uterus can cause leg cramps or sharp pains down your leg.
We recommend you to:
- Drink plenty of fluids (at least 10 to 12 glasses a day)
- Avoid food rich in salt
- Elevate your legs and feet while sitting. Avoid crossing your legs
- Wear comfortable, low heeled shoes
- Maintain a protein rich in calcium diet (milk broccoli, cheese, etc.)
- Notify your health care provider if your hands or face swell, this might be a warning sign of preeclampsia or toxemia, a pregnancy related high blood pressure
- Avoid lying on your back, since the weight of your body and the pressure of your enlarged uterus can slow the circulation in your legs, causing cramps
- Try massaging the cramps or apply heat pads to the sore area
- Avoid standing for long periods, sit with the feet up and rotate the ankles regularly, gently flex feet to stretch calf muscles, lie down with legs elevated
- Sleep on the left side
- Wear compression socks
- Physical activity, if possible, is recommended every day: take walks, swim or walk in the pool, (the physician will recommend the exercises’ length and intensity)
B. Healthy diet
For a healthy pregnancy you should follow a healthy diet.

Familiar with the sentence “you need to eat for two”? In fact, exclusive breastfeeding requires only an additional 300 to 500 calories per day to produce the milk after pregnancy. These requirements could be reached by simply adding 2 small healthy snacks to your diet.

Folate is a B-vitamin naturally present in some foods (vegetables, fruits, nuts, beans….). It is also available as a dietary supplement to be added to foods. It has a role in DNA formation and cell division.
A deficiency during pregnancy can lead to the development of birth defects such as:
– Neural tube defects
– Congenital heart defects
– Oral facial clefts
START the supplementation early if you are planning to get pregnant!

i. Diet recommendations
Healthy and balanced diet:
- Food: rich in fiber, and include a variety of vegetables and fruits, like carrots, cooked greens, bananas, and melons, including beans and whole grains
- Vegetables and fruits: at least 6 servings per day
- Calcium intake: 4 dairy products to prevent bone problems in the future
- Protein intake: animal or vegetable iron (100g) or supplements, to prevent anemia
- Fluids: water (at least 8 – 10 glasses per day), including fresh juice, soups, herbal tea, and sparkling water instead of soda
- Caffeine intake: maximum 2 cups of coffee or tea per day
- Vitamins: with iron and folic acid every day (prescribed by your physician)
حمض الفوليك ضروري، إبتداءً من 1-3 أشهر قبل وأثناء الحمل، لمنع التشوّهات الخلقية مثل “السنسنة المشقوقة” ، من خلال:
Avoid:
- Soft cheese (like feta, Brie and goat cheese)
- Raw meat and fish (sushi)
- Smoking or being around smokers
- Alcohol
- Fish that contain high levels of mercury
Please note that cheese, milk and juice should be pasteurized.
Pregnant women with toxoplasma negative should follow the same diet recommendations as toxoplasma positive women with one additional precaution, soak fruits and vegetables in a diluted disinfectant solution, then rinse with bottled water thoroughly before cooking/eating, to remove all traces of soil.
It is advisable to monitor ones diet during breastfeeding and avoid the following:
- Sweets and sugar: because they contain artificial sugar
- Food that can cause gas: onions, garlic, cauliflower, radish, beans (lentils, chickpeas…), because they might cause colic and discomfort for the baby
- Dieting while breastfeeding, unless it was critical under a dietitian’s supervision, because it might affect your milk supply
It is also important to check with a nutritionist during all pregnancy stages and breastfeeding.
C. Exercise
Pregnancy is an ideal time for positive lifestyle modifications, including increasing physical activity (if possible) and consuming a healthier diet.
If your pregnancy is normal with no complications, doctors recommend at least 15 to 20 minutes of daily physical activity. This can improve your posture and decrease some normal pregnancy discomforts such as backaches, constipation, bloating, swelling and fatigue. It can improve your mood and assist you to have a better sleep. You are allowed to do safe, mild to moderate exercises at least 3 times a week unless your physician advised otherwise.
It is not advised to exercise in case you are experiencing:
- Vaginal bleeding or spotting
- Low placenta
- Weak cervix
- Premature rupture of membranes
- Previous premature births or early labor history
Can do:
- Swimming
- Brisk walking
- Indoor stationary cycling
- Prenatal yoga
- Low-impact aerobics
Avoid:
- Contact sports (softball, football, basketball and volleyball…)
- Any exercise that might cause abdominal trauma
- Activities that require extensive jumping, hopping, skipping, bouncing or running
i. Kegel exercises
Kegel exercises (pelvic floor exercises) help strengthen the muscles that support the bladder, uterus and bowel.
By strengthening these muscles during pregnancy, you can develop the ability to relax and control the muscles in preparation for labor and birth.
Kegel exercises are highly recommended after delivery to promote the healing of perineal tissues, increase the pelvic floor muscles strength, and help these muscles return to a healthy state, including urinary control.
How to do Kegel exercises?
- Tighten your pelvic floor muscles for 10 counts then relax for 10 counts
- Repeat 10 times for 3 times a day (morning, afternoon and evening)
- Please note that you should not perform this exercise while urinating
D. Discomfort tips
| Discomfort | Recommendation |
| Abdominal pain and discomfort Sharp, shooting pains on either sides of the stomach. These pains might also move to your thigh and leg. |
|
| Round ligament pain Sharp pain in the abdomen or hip area on one or both sides, may extend to the groin area (most common during the second trimester) |
|
| Muscle tightening The muscles in the uterus will tighten causing irregular and infrequent contractions, starting from the 4th month of pregnancy |
|
| Backaches Usually caused by the strain put on the back muscles and posture changes |
|
| Digestive complications Constipation caused by your hormones, vitamins and iron supplements and the pressure on your rectum from your uterus |
|
|
Hemorrhoids are swollen veins that appear as painful lumps on the anus, result from increased circulation and pressure on the rectum and vagina from your growing baby |
|
|
Heartburn and indigestion is a burning feeling, during pregnancy, which starts in the stomach and rises to the throat caused by the slow mechanism of your digestive system due to changing hormone levels. Also, by your enlarged uterus that crowds the stomach, pushing stomach acids upwards |
|
|
Nausea and vomiting can occur at any time of the day but might be worse in the morning on an empty stomach – morning sickness or if you are not eating enough. It is caused by hormonal changes, most often occurs early in pregnancy until your body adjusts to the increased production of hormones |
|
| Sleeping difficulties Finding a comfortable resting position can become difficult later in pregnancy |
|
| Dizziness Caused by hormone levels changes and blood volume, stress, fatigue, and eyestrain |
|
| Fatigue Your growing baby requires extra energy, which might make you feel tired |
|
| Headaches How often headaches occur and how bad they are can vary. |
|
| Frequent urination During the first trimester, the growing baby presses against the bladder, causing a frequent need to urinate. This will happen again when the baby’s head drops into the pelvis before birth |
|
| Vaginal discharge Increased blood supply and hormones cause your vagina to increase normal secretion. Normal vaginal discharge is white or clear, non-irritating, odorless, and might look yellow on your underwear or panty liners |
|
E. Sex
Sex is definitely allowed, there is no reason to change your sexual activity during pregnancy, unless your physician advises otherwise.
Intercourse and orgasm during pregnancy will not harm your baby in any way, unless you have a medical problem.
Your physician might recommend not having sex early in pregnancy if you have a history of miscarriages. Intercourse might also be restricted if you have certain pregnancy complications, such as preterm labor or bleeding.
F. Airline travel

The safest time to travel when you are pregnant is during your second trimester (18-24 weeks). Hence, if you want to enjoy your holiday trip, make sure to do the following:
– Check with the airline for its requirements before you book
– Consult your physician first and carry written documentation of your due date
– Wear seatbelt strap over lower lap/upper thighs
– Choose an aisle seat and walk when possible
Commercial airline travel is generally safe for women with uncomplicated pregnancies. Usually fetal heart rate is not affected during flight, although airlines’ individual policies may vary. Consult our physician for approval before travel.
Advice:
- Maintain hydration
- Periodically move lower extremities
- Use compression stockings
- Avoid tight clothing
- Wear seat belt continuously to prevent unexpected turbulence injury
Part 2: Pregnancy stages and recommendations
A. First trimester: (1 to 15 weeks pregnant)
i. First medical visit
The first medical visit is for determining general health and inform your physician about all the risks that might affect your pregnancy. First visit usually take longer than future ones, to determine:

Congenital heart defects can arise from a genetic disorder, pregnancy complications, or unknown causes. If pregnant, consider:
– Nutritional guidance
– Ultrasound screenings
– Medications monitoring during pregnancy

1 in 100 newborn has a heart defect which can be diagnosed prenatally.
Get the mid-pregnancy ultrasound scan performed today by a maternal-fetal-specialist to detect any possible congenital anomalies.
Reduce pregnancy infections risk:
– Wash hands with soap and water frequently
– Avoid touching saliva and urine from young children
– Avoid unpasteurized (raw) milk
– Avoid touching or changing dirty cat litter
– Get tested for Sexually Transmitted Diseases (STD)
Most importantly, consult your doctor regularly! For more information, contact us on +961 5 957 000 ext 15500

Spina bifida is a neural tube defect developed during the first month of pregnancy leaving the spinal cord partially open. This might lead to minor physical problems or severe physical and mental disabilities, including loss of muscles, nerve functions and sensations. Its risk can be reduced by 70% by getting an early screening through:
– The triple test
– The alpha-fetoprotein test
Adequate folic acid intake of 400 micrograms per day before and during pregnancy can help prevent the development of this condition.

Birth defects arise early in pregnancy and they can be detected as early as during the first trimester of pregnancy by prenatal ultrasounds and chorionic velocity sampling or later on with amniocentesis all available MLH.
- Due Date
- Health History
- Family’s medical history
- Pregnancy risk factors based on age, health and/or personal and family history
You should notify your physician about any medication taken or currently taking.
ii. Lab tests
In the first trimester your physician will order many lab tests including:
- Complete Blood Count (CBC)
- Rubella – immunity test (German measles)
- Toxoplasma – immunity test (Toxoplasma gondii parasite)
- HBSAG – hepatitis B (liver infection)
- Urinalysis – kidney infection and bladder infection
- Blood type and Rh factor screening – protein causes an immune system response.
Follow-up visits are recommended every:
- 4 weeks until 28 weeks
- 2 to 3 weeks from 28 to 36 weeks
- Weekly from 36 weeks until delivery
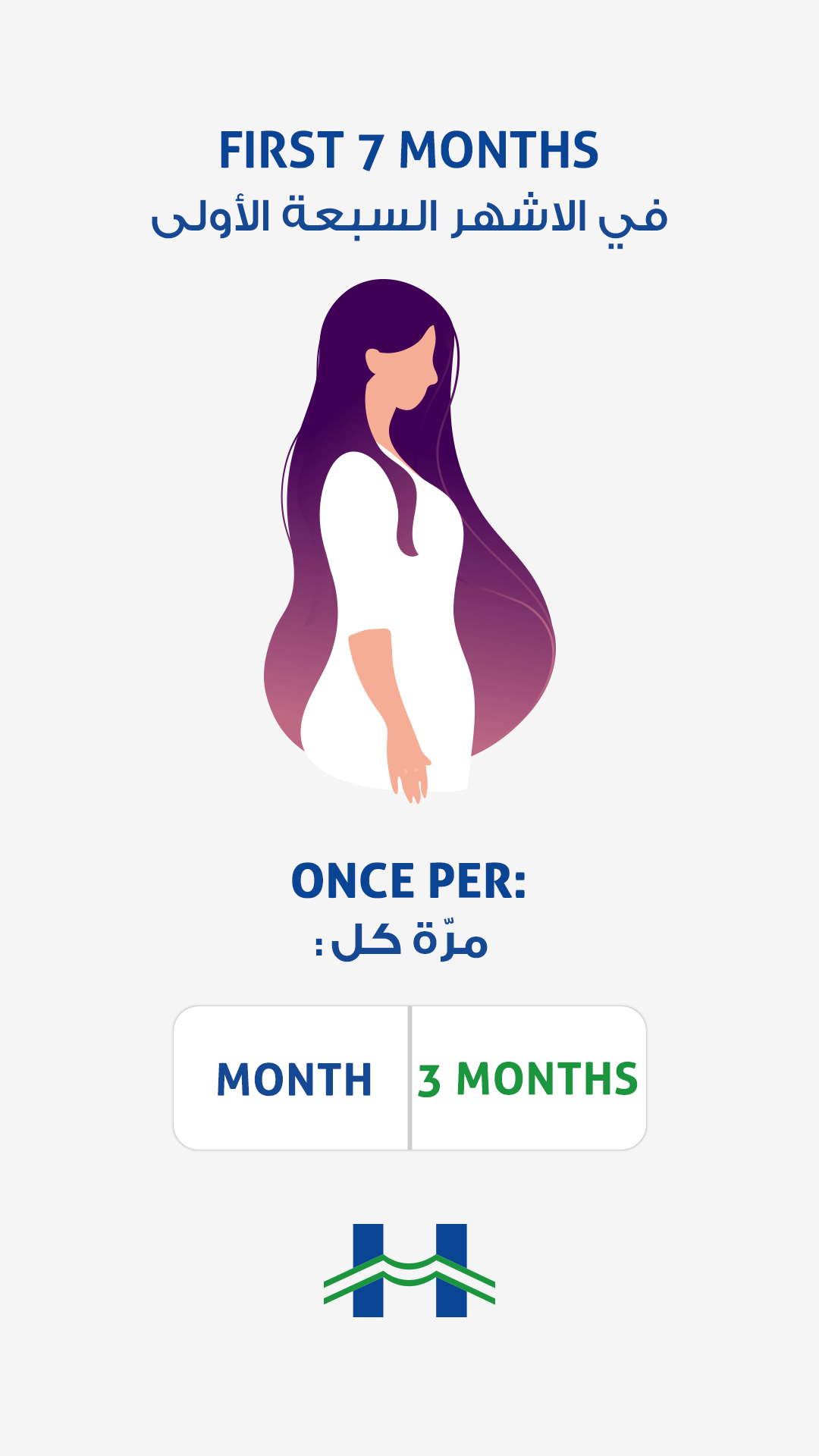
For a healthy pregnancy regular medical visits are required:
– Before 28 weeks (7 months): Monthly
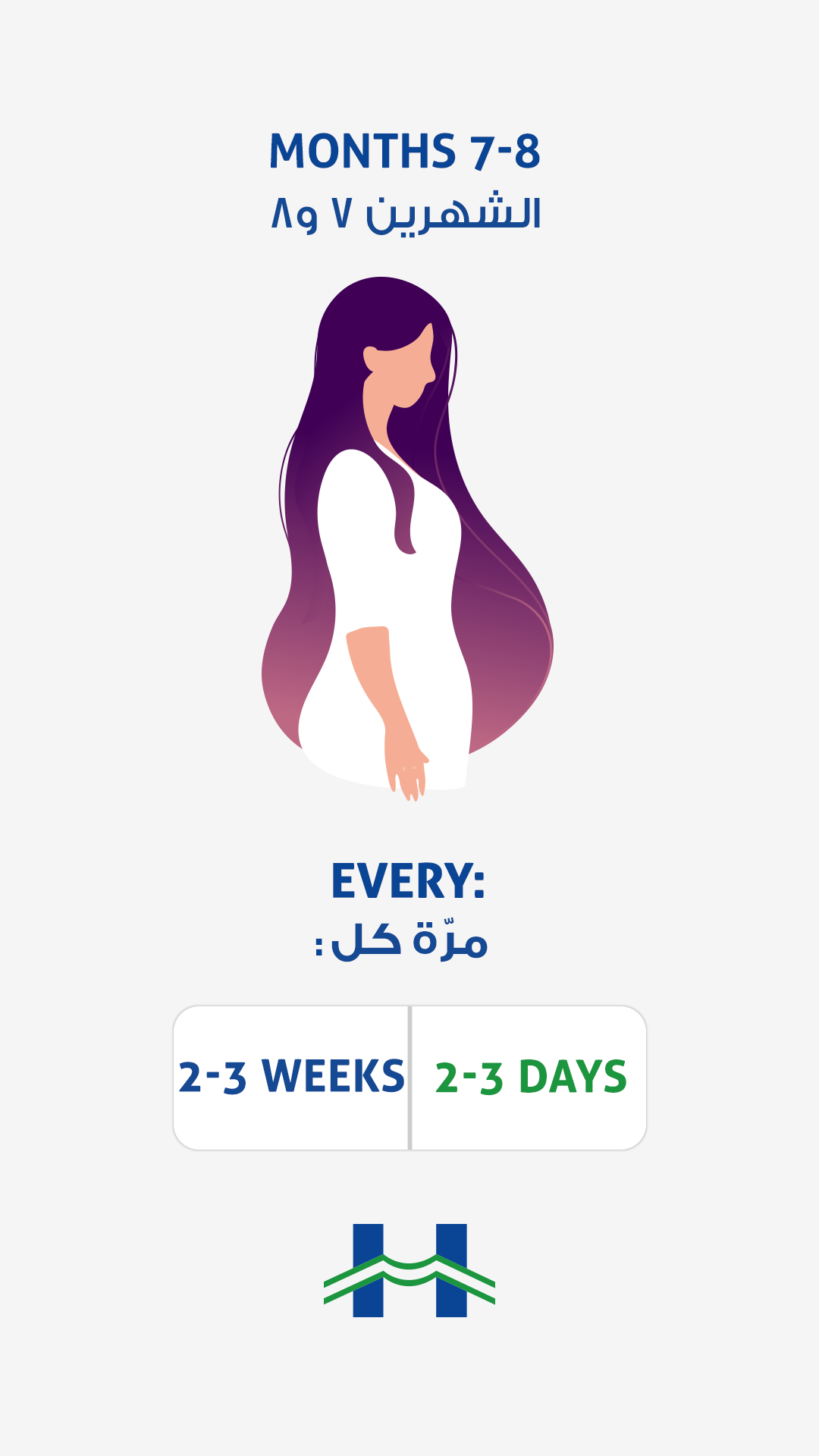
For a healthy pregnancy regular medical visits are required:
– Weeks 28 to 36 (7-8 months): Every 2-3 weeks
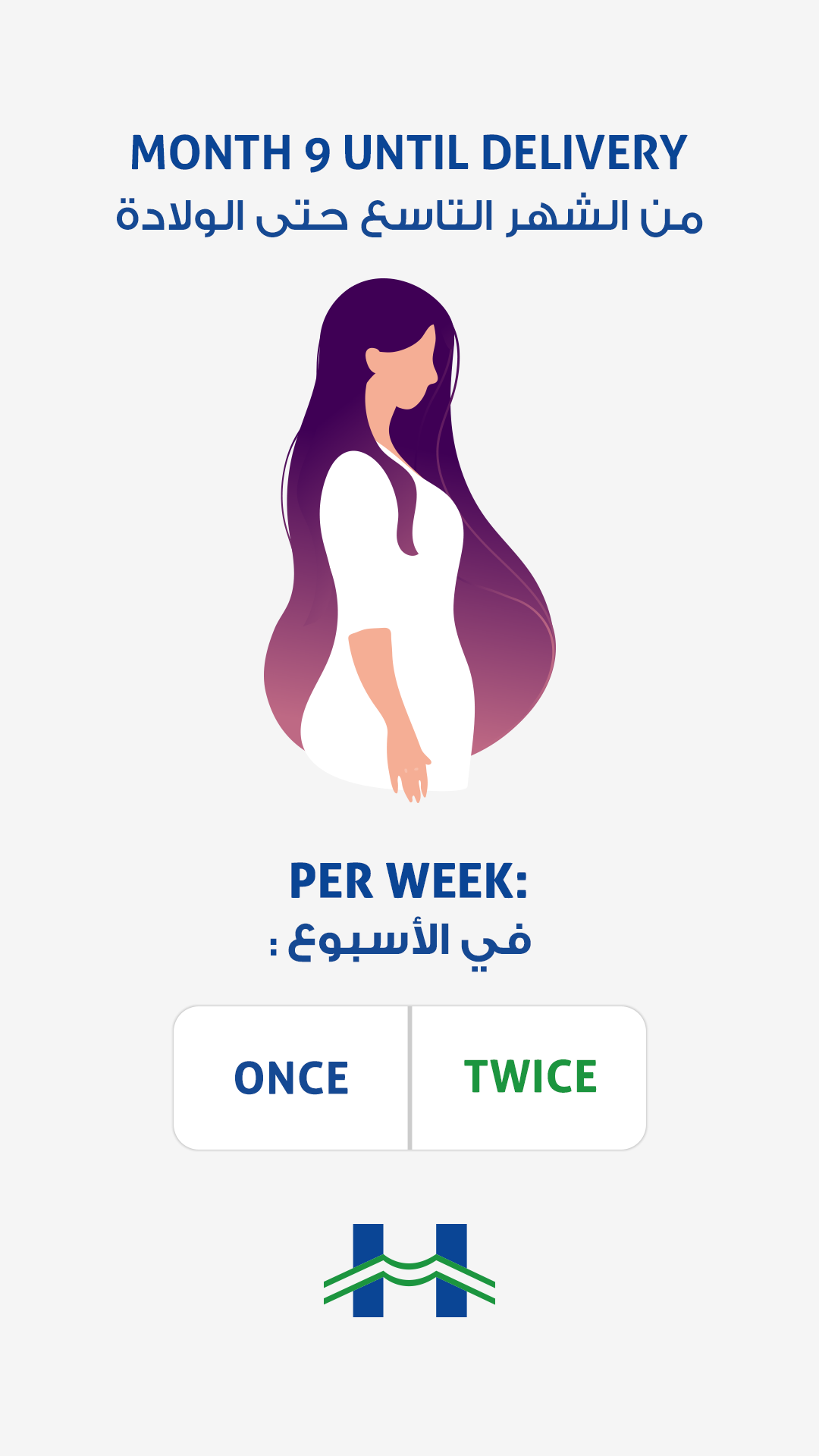
For a healthy pregnancy regular medical visits are required:
– Week 36 (9th month) until delivery: Weekly
iii. Non Invasive prenatal testing – NIPT

Ensure a healthy pregnancy with NIPT.
– A highly recommended non-invasive prenatal genetic test
– Analyses the baby’s DNA to detect chromosomal abnormalities and syndromes.
– It’s only a quick and harmless blood test
*The best time to undergo NIPT, without any risk, is between the 11th and 12th week!

Early pregnancy screening can detect fetal chromosomal anomalies. The latest NIPT (Non-Invasive Prenatal Test) is among the most innovative and advanced pregnancy screening techniques. Dr. Emma Abboud, Head of the medical laboratory at MLH tells us more about this blood test.
NIPT a non-invasive blood test that can detect approximately 99% of fetuses with Down syndrome and Trisomy 18, and up to 92% of fetuses with Trisomy 13, and saves the mother from undergoing other invasive tests. NIPT is recommended when:
- Depending on the woman’s age and the physician’s prescription
- Abnormal findings on ultrasound
- Previous history of a chromosome anomaly

MFM specialists: for the next generation’s health! Clink on the link in the bio to read the full article
B. Second trimester: (15 to 28 weeks pregnant)
i. Rh factor testing
Rh is an antigen protein found in most people’s red blood cells. If you are Rh- (negative) then you will be given a Rh immune globulin injection, during the 28th week of your pregnancy, to prevent harmful antibodies development. In case your baby is Rh+, after delivery, you will also be given a similar injection.
ii. Oral glucose challenge testing
This test involves rapidly drinking a sweetened liquid, containing 50 grams of glucose. 60 minutes after, a blood test is done to measure how the glucose solution was processed by the body. This test is performed usually between week 24 and week 28 of pregnancy. If the physician is concerned about gestational diabetes he might conduct this test earlier.


iii. Triple screen test
The triple screening is a blood test usually done at 15 to 20 weeks of pregnancy.
Its purpose is to detect if the baby is at high risk of certain birth defects.
iv. Morphology scan
A detailed ultrasound scan that inspects your baby’s body and observes the position of the placenta, the umbilical cord, the amniotic fluid around your baby, and your uterus and your cervix. It is also known as an anomaly scan or a 18-20 week scan.
The doctor will measure the baby’s full body to confirm the expected delivery date and often tells the baby’s sex, with about 95% accuracy. He will also check for growth or development anomalies in the heart, stomach, kidneys and limbs.
C. Third trimester: (29 to 41 weeks pregnant)
In the third trimester medical visits will mostly increase, your visits will increase to one per week as your physician will ask for more ultrasounds, blood tests, urine analysis and a Pap smear test screening – if you are planning for a normal vaginal delivery. In the last few weeks of pregnancy you will be put on a monitor, this will allow the physician to monitor the baby’s pulse, movements in the womb and contractions (if applicable).
i. Non-Stress testing
NST measures baby’s heart rate in response to the baby’s environment. Two belts will be placed on the abdomen; one has sensors to measure the fetal heart rate and the other detects uterine contractions. The baby’s movement will be counted as well. Most babies have a sleep/wake schedule of 20 to 40 minutes in the womb.
ii. Baby movements count
Baby’s regular movements are a sign of good health. Though babies may sleep for up to an hour, most of the time the baby is active and moving. On average, a healthy baby kicks or moves at least six to 10 times within one hour.
Contact your physician immediately if you experience noticeable changes in the baby’s movements after 28 weeks (less than 6 to 10 movements per hour).
iii. Signs of premature labor: (before 36 weeks pregnant)

According to the WHO, 15 million babies are born preterm every year with a 7% mortality among children under the age of 5. It mostly occurs spontaneously for a variety of reasons, including:
– Multiple pregnancies (twins, triplets…)
– Infection and chronic conditions like diabetes and hypertension
– Complications during pregnancy
– Genetic predisposition

Preterm labor can affect ANY pregnancy. However, some risk factors include:
– Previous preterm delivery
– A multiple pregnancy
– Tobacco use and substance abuse
– Less than 18 months between pregnancies
- Four or more contractions or tightening of the muscles in the uterus in one hour that do not go away after changing your position or relaxing
- Regular constant, irregular tightening, or low dull pain in your back (is not relieved after any comfort measures)
- Pressure in the pelvis or vagina
- Lower abdominal cramping that might feel like gas pain (with or without diarrhea)
- Persistent menstrual-like cramps
- Increased vaginal discharge
- Fluid leaking from the vagina
- Vaginal bleeding
iv. Hypertension / Preeclampsia signs
- Headache
- Vision problems
- Pain in the upper abdomen
- Sudden weight gain
- Consult your physician
D. Preparing baby’s room
- Clean all surfaces using an infant formulated detergent:
1- Room
2- Walls
3- Floor
4- Crib
5- Furniture
- Crib
1- Less than 10 years old
2-Not broken or modified
- Mattress
1- Firm
2- 2 fingers width
3- Fitted protection pads
4- Sheets, all washed and ironed.
- Install a changing table (bathtub included)
- Set up and test a baby monitor and keep the receiver close
- Wash and iron all the baby clothes before organizing the closet
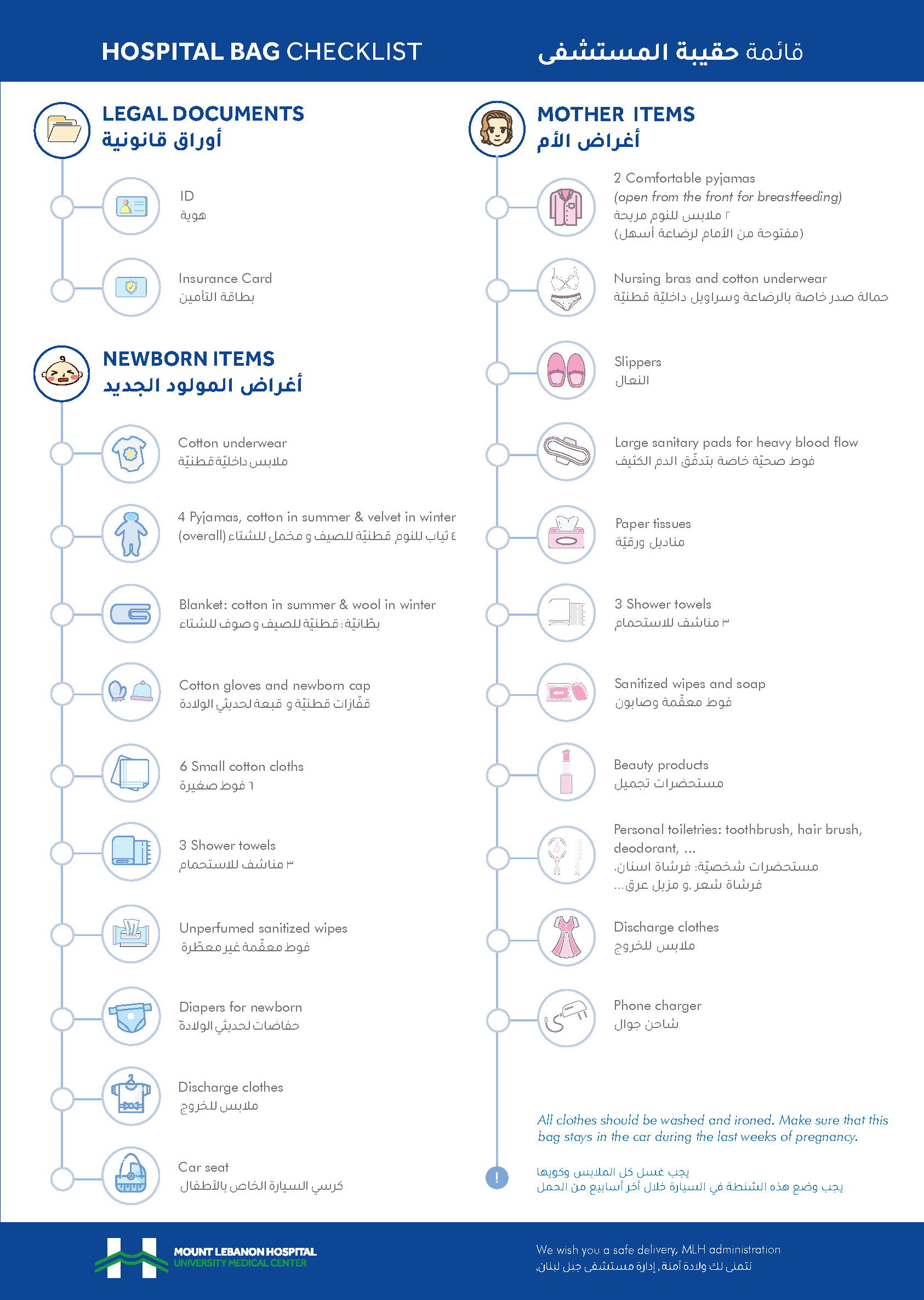
E. Hospital bag checklist
Part 3: The Big Day (labor and delivery stages)
A. Labor
i. True or false labor
False labor:
- Contractions are often irregular and do not get closer together
- Contractions might stop when you walk, rest or might even stop when you change position
True labor:
- Contractions come at regular intervals and get closer together as time goes on. True labor contractions become longer, stronger and more intense (last about 30 to 70 seconds each)
- Contractions continue, despite moving or changing positions
Tips to ease true or false labor contractions and discomforts:
False labor:
- Change position or activity
- Drink enough fluids (at least 10 to 12 glasses per day)
- Rest and relax
True labor:
- Try to distract yourself: take a walk, go shopping, and watch a movie
- Soak in a warm tub or take a warm shower. Ask a physician if you should take a tub bath if your water has broken already
- Try to sleep (if at evening time). You need to save energy for labor
It is essential to call your physician when you have:
- Bright red vaginal bleeding
- Continuous leaking of fluid or wetness, or if your water breaks (fluid gushing)
- Strong contractions every five minutes for one hour
- Unable to “walk through” contractions
- Noticeable change in baby’s movement (less than 6 to 10 movement in one hour)
ii. Labor Signs
Labor begins when the cervix starts to dilate. The muscles of the uterus contract at regular intervals. During contractions, the abdomen becomes hard. Between contractions the uterus relaxes and the abdomen becomes soft.
Some women experience very distinct labor signs, others don’t. No one knows what causes labor to start, but several hormonal and physical changes might indicate the beginning of labor.
- Lightning:
The process of your baby settling or lowering into the pelvis is called lightning. It can happen a few weeks or a few hours before labor. Because the uterus rests on the bladder more after lightening, you might feel the need to urinate more frequently.
- Mucus plug:
The mucus plug accumulates at the cervix during pregnancy. When the cervix begins to open wider, the mucus, clear, pink or slightly bloody, is discharged into the vagina. Labor might begin soon after, the mucus plug is discharged or one to two weeks later.
- Contractions:
Contractions come at regular intervals and increase in frequency, duration and intensity over time.
As time progresses, the contractions come at closer intervals.
This part of the first stage of labor (latent phase) is best experienced in the comfort of your home.
Contraction timing:
Record the time at the beginning of one contraction and again at the beginning of the next one.
- Time between contractions includes:
- Contraction duration (length),
- Minutes (interval) between one and the other.
Mild contractions generally begin 10 to 15 minutes apart. The contractions become more regular until they are less than five minutes apart. Active labor (time you should go to the hospital) is usually characterized by strong contractions that are 3 to 4 minutes apart.
- Amniotic membrane rupture:
The rupture of the amniotic membrane, which is the fluid -filled sac that surrounds the baby during pregnancy, also referred to as your “water breaking”.
It might feel either like a sudden gush of fluid or a drip of fluid that leaks steadily. The fluid is usually odorless and might look clear or straw-colored.
If your “Water Breaks”:
- Contact physician and go to the hospital’s maternity department right away
- Record the time it happened, the color and odor of the fluid
- Labor might or might not start soon after water breaks
It is also common to be in labor without the water breaking.
Cervix effacement and dilation:
Your cervix gets shorter and thins out in order to stretch and open around your baby’s head. The shortening and thinning of the cervix is called effacement and is measured in percentages from 0% to 100%. The stretching and opening of your cervix is called dilation and is measured in centimeters from 1 to 10 centimeters.
Effacement and dilation are a direct result of effective uterine contractions. Progress in labor is measured by how much the cervix has opened and thinned to allow your baby to pass through the vagina.
B. Choices of pain management during labor
The way contractions feel is different for each woman and might feel different from one pregnancy to the next.
There are many choices of pain management during labor such as:
Non-medicated Pain Management:
Relaxation: This technique can improve your ability to detect and release tension.
Touch: Gentle massage or light stroking, on the back, shoulders, hands and legs to relieve tension.
Hot or cold therapy: A warm towel or a cold pack may help relax tense or painful areas.
Breathing: Techniques using different breathing patterns and types to help direct the mind away from discomfort.
Positioning and movement: Many women find that changing positions and moving around during labor helps to relieve discomfort and may even accelerate the process.
Medicated pain management:
The anesthesiologist decides with the physician which type of pain management is to be used, based on the patient’s case and labor stage, while monitored through the whole procedure.
Epidural anesthesia: Numbing medications infused through a thin catheter, inserted into the space that surrounds the spinal cord in the lower back, causing a loss of sensation in the lower body. Infusions of medications may be increased or stopped as needed. This type of anesthesia is used during labor, vaginal and cesarean deliveries.
Spinal anesthesia. A single dose of the anesthetic agent directly injected into the spinal fluid. It acts very quickly and causes complete loss of sensation and loss of movement in the lower body. Often used for cesarean deliveries.
General anesthesia. Often used in emergency cesarean deliveries, this type of pain relief involves administering an anesthetic agent that causes induced sleep.
C. Normal vaginal delivery
Normal Vaginal Delivery is the most common type of birth.
i. First Stage
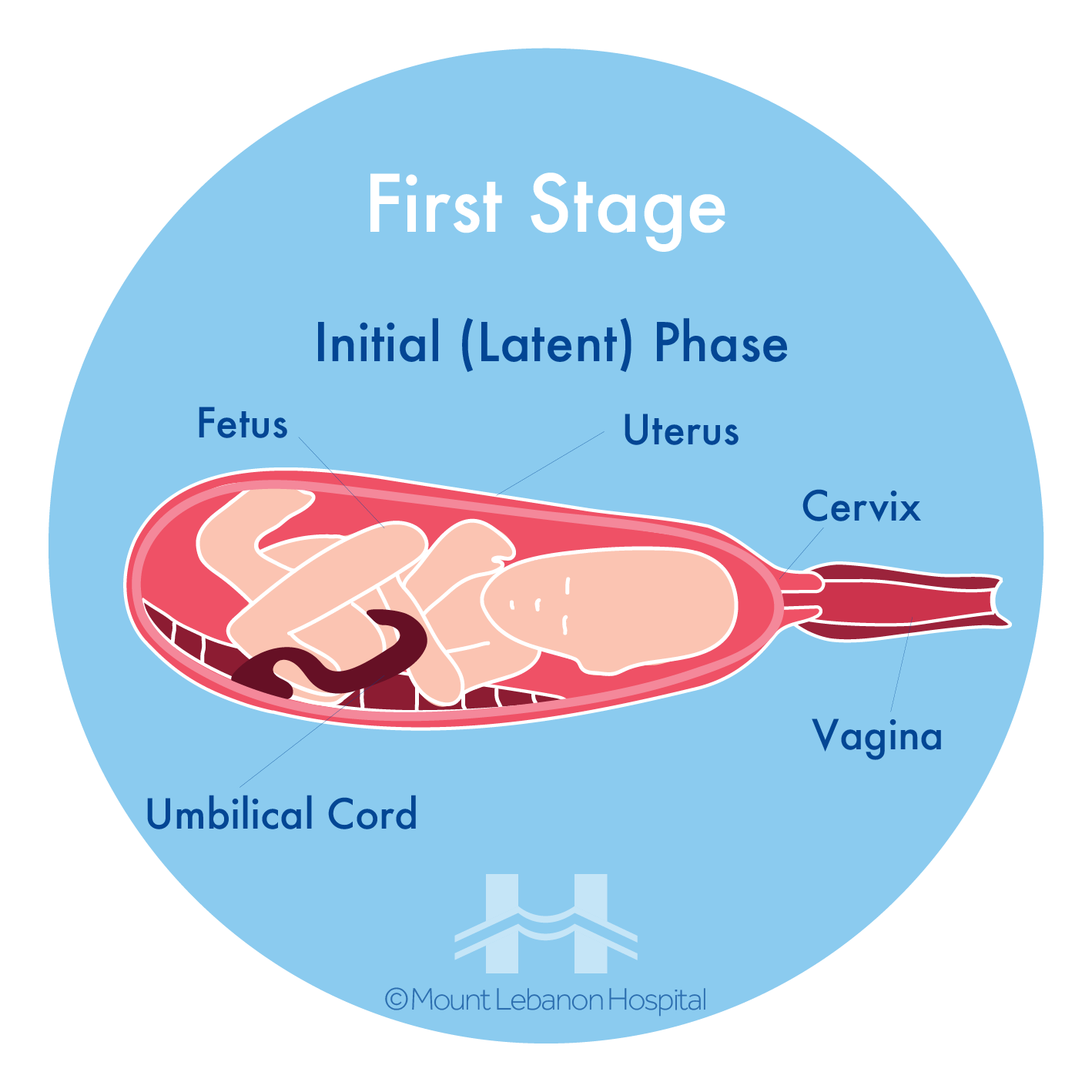
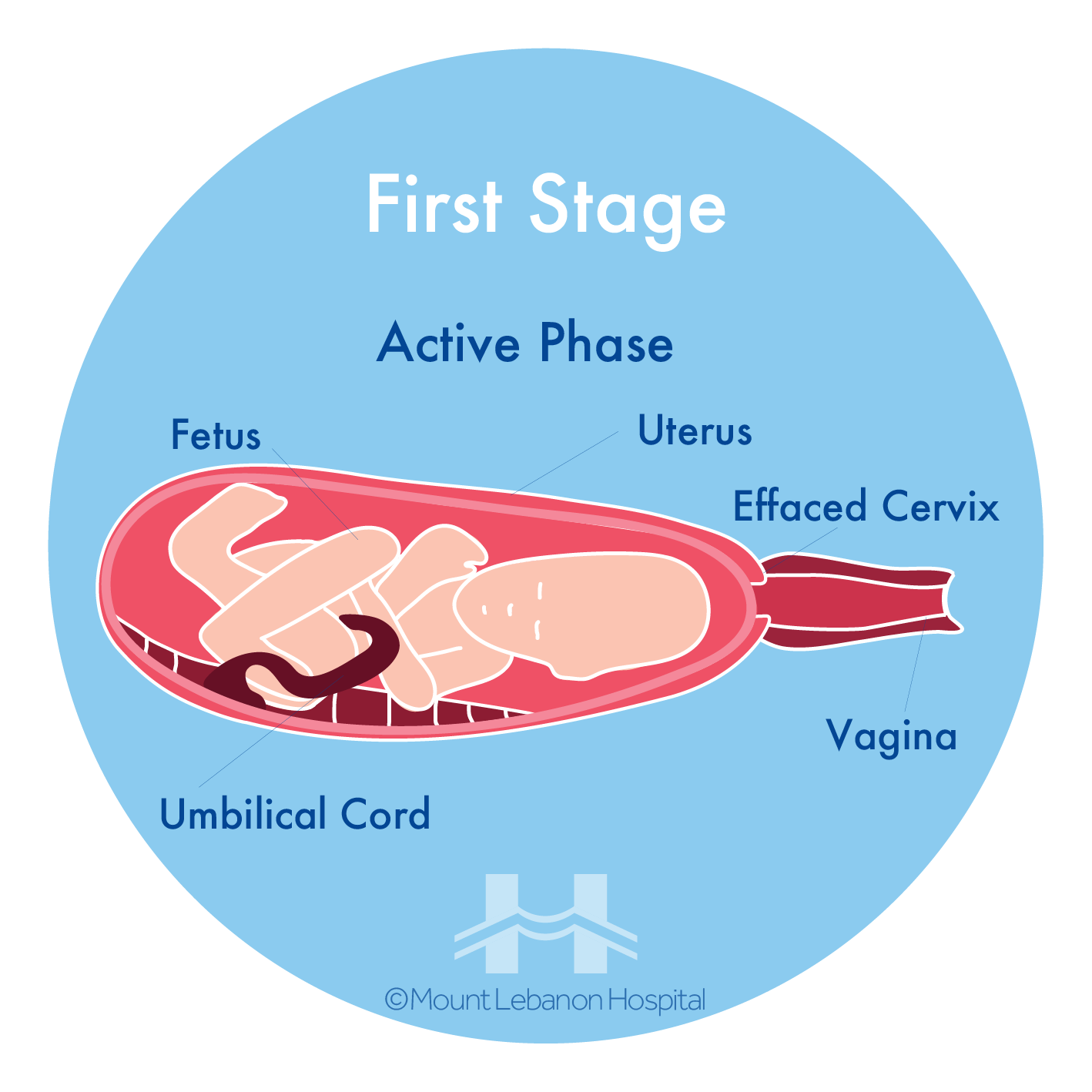
The body is preparing to give birth, with signs such as:
- Regular, painful, stronger and more frequent contractions
- Cervix is opening and getting ready for the baby to go through
- Backache
- Water breaks
ii. Second Stage
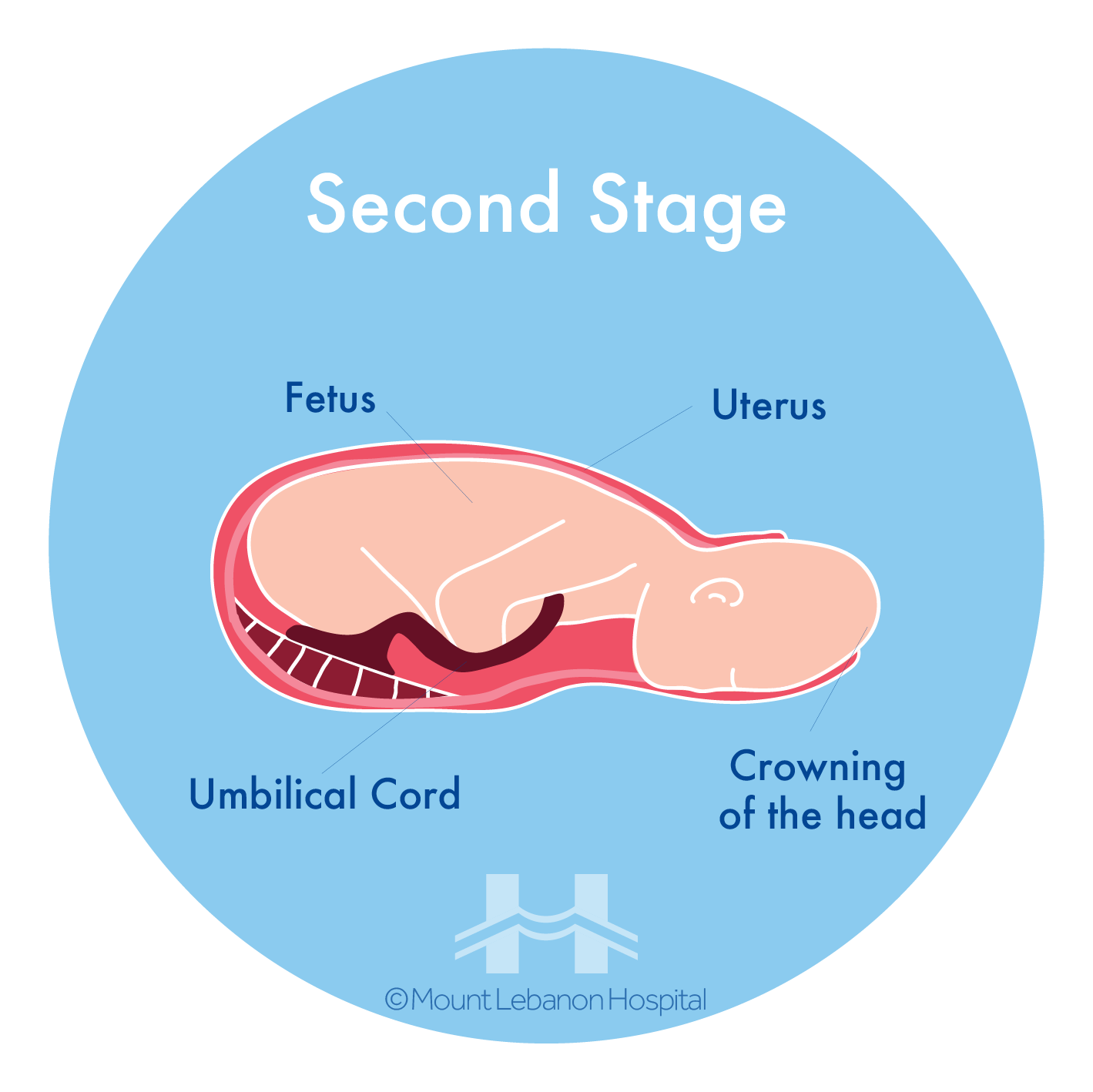
The woman is giving birth to the baby.
- The midwife will help to find a comfortable position;
- Take deep breaths;
- Start to push, when the cervix is fully dilated, and when the midwife or doctor tells you to during contractions;
- Give several pushes until the contraction ends;
- After each contraction, rest and get your strength up for the next one;
- The baby’s head moves down the vagina until it can be seen;
- The doctor helps with the baby’s head;
- The father cuts the umbilical cord after the doctor places 2 clamps.
iii. Third Stage
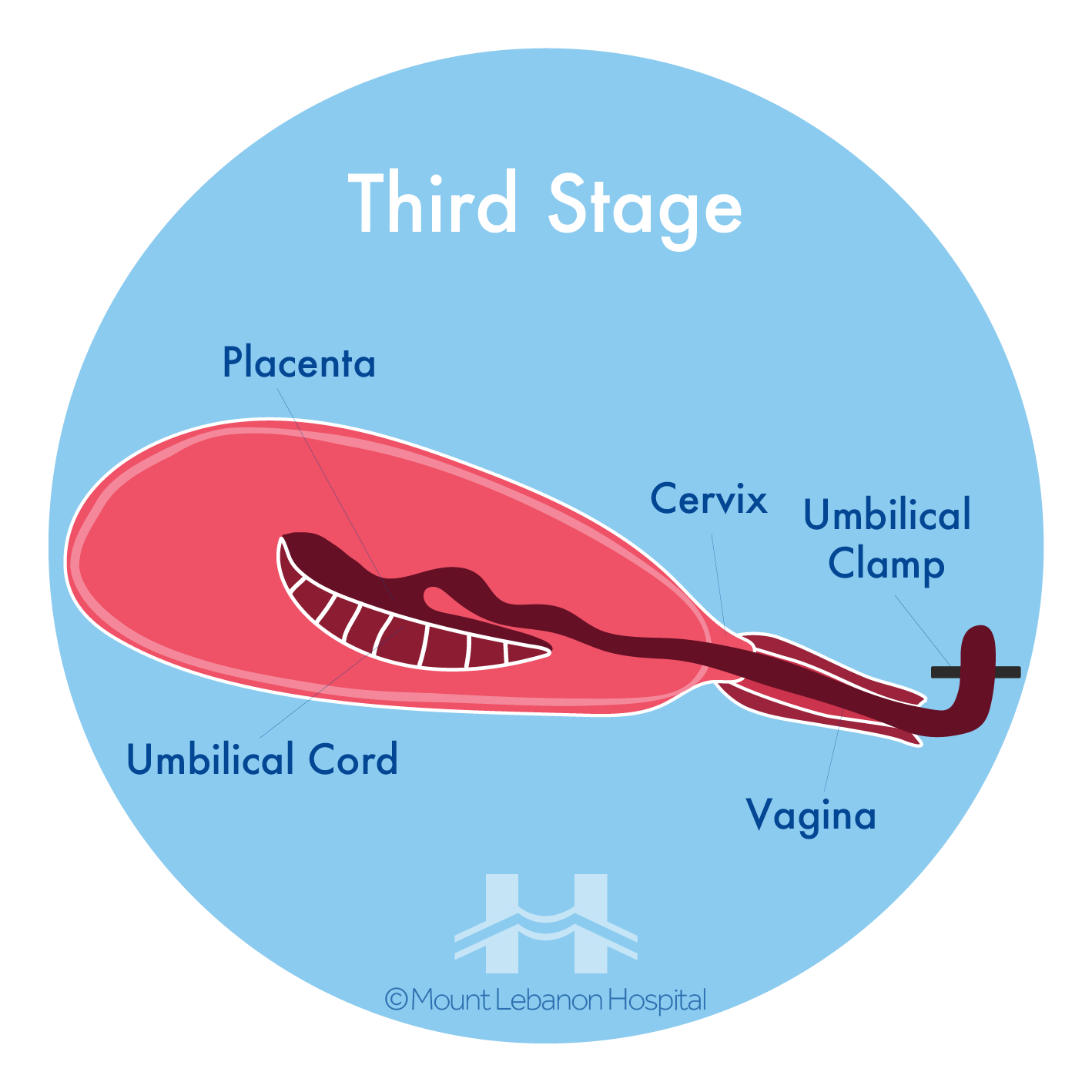
After the birth of the baby:
- Placenta is delivered
- The women will be injected with a drug called oxytocin which makes the womb contract
- Helps to prevent heavy bleeding known as “postpartum hemorrhage”
While labor can be a straightforward, uncomplicated process, it might require the assistance of the medical staff. This assistance can vary from use of medicines to emergency procedures. Such as the following:
Episiotomy: A surgical incision made in the perineum (the area of skin between the vagina and the anus). The incision enlarges the vaginal opening to allow the baby’s head to pass through more easily and to prevent tearing of the mother’s skin.
Amniotomy “water breaking”:
The artificial rupture of the amniotic sac, which contains the fluid surrounding the baby. Amniotomy can be done either before or during labor, and usually done to induce or augment labor.
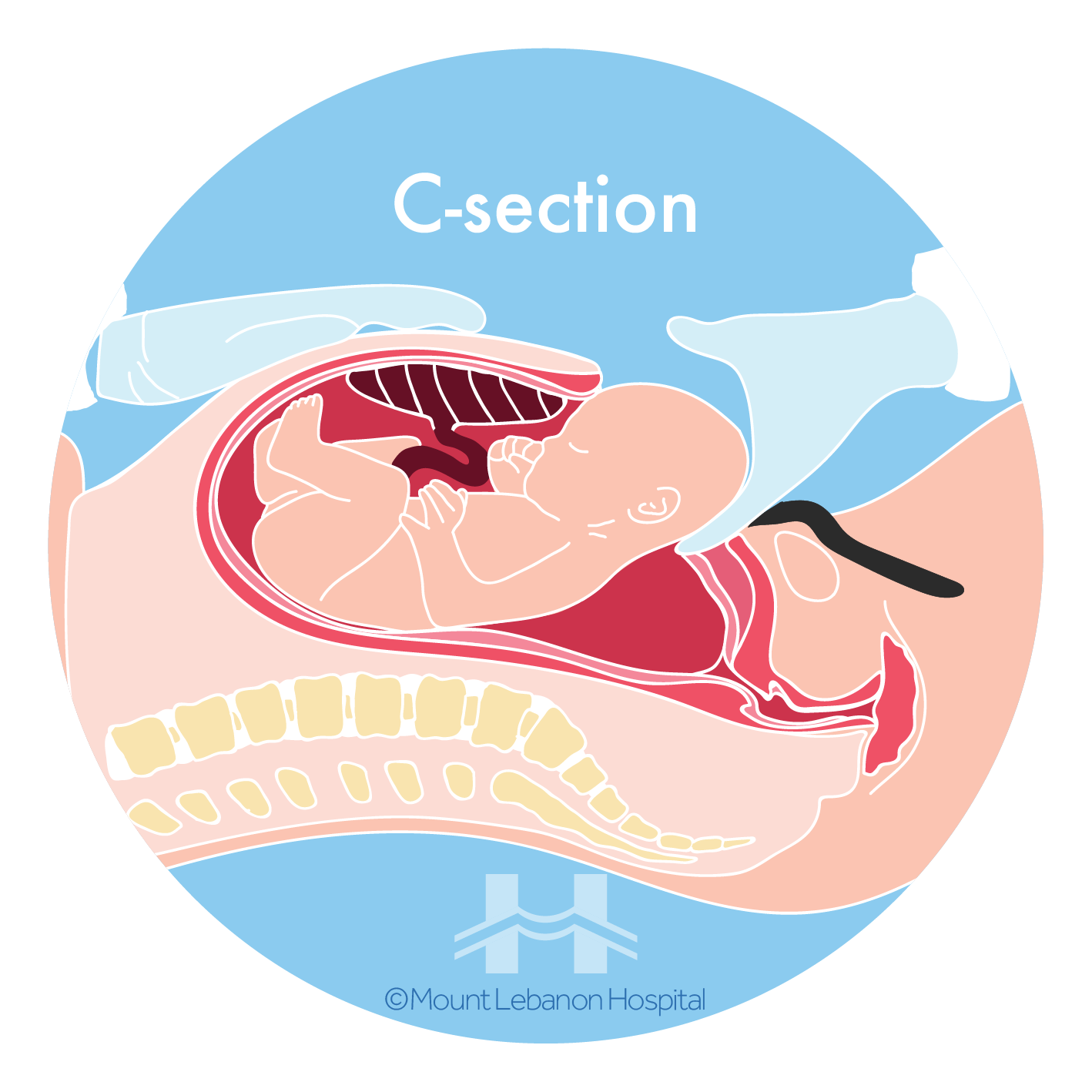
D. Cesarean delivery (C-section)
Also called a C-section, is a surgical procedure performed if a normal vaginal delivery is not possible. During this procedure, the baby is delivered through surgical incisions made in the abdomen and the uterus.
Factors that can affect whether a planned or unplanned C-section is needed if following conditions apply:
- Cephalopelvic disproportion (CPD)
- Previous cesarean birth
- Multiple pregnancy
- Placenta previa
- Traverse lie
- Breech presentation
- Failure of labor to progress
- Cord compression
- Prolapsed cord
- Abruptio placentae
- Abnormal fetal heart rate during labor
What to expect before a C-section?
- You will be asked if you consent to the procedure, and in some cases might be asked to sign a consent form
- The anesthesiologist will discuss the type of anesthesia to be used
- A heart, pulse and blood pressure monitor is applied
- Hair clipping will be done around the incision area
- A catheter will be inserted to keep the bladder empty
- Medicine will be administered directly by IV
E. Skin to Skin
Right after the baby is born, skin to skin contact is recommended. This is done by placing the baby belly-down directly on the mother’s chest, for the first hour. This will allow the mother and baby to get to know each other.
If the baby needs to meet the pediatrician first, or after a C-section, the mother can unwrap the baby and conduct skin to skin contact shortly after birth.
Newborns require skin-to-skin contact, but it is also sometimes overwhelming for new moms, therefore it’s okay to start slowly after the mother regains her strength and is ready for this step.
Part 4: Guide for Mom and Newborn
A. 24-Hour rooming-in: Rest is healing
Benefits for the mother:

More than 10% of women suffering from Baby blues experience more severe and persistent sadness even if their baby is healthy. In postpartum depression, the baby’s well-being may become at risk since a depressed mother may have trouble enjoyng, bonding with, and caring for her infant
- Better quality of sleep
- Increased confidence in handling and caring for the baby
- Ability to learn what your baby’s cues are sleepy, stressed, in need of quiet time or hungry
- Identification of early feeding cues: rooting, opening mouth and sucking on tongue, fingers or hand
- Improved breastfeeding experience
- Less infant crying and distress
- Less “baby blues” and postpartum depression
- Parents are better-rested and more relaxed by the end of the first week home
- Increases opportunity for skin-to-skin contact
Benefits for the baby:
- Better quality of sleep
- More stable body temperatures
- Generally more content
- Stable blood sugar
- Breastfeed longer and easily
- Lower levels of stress hormones
B. Breastfeeding

Your Daily Intake: Did you know that breastfeeding benefits mothers too?
– It helps the uterus return to its pre-pregnancy size and reduces post-delivery bleeding.
– It makes it easier to lose the pregnancy pounds.
– It may reduce the risk of postpartum depression and breast and ovarian cancer.
– It can delay the return of the menstrual period.
It saves money.

Moms should breastfeed for their health and their baby’s:
– Rich in carbohydrates, proteins, fats, and vitamins
– Rich in antibodies, to prevent illnesses
For moms:
– Reduces postpartum depression

Kangaroo care is the practice of skin-to-skin contact between infant and parent which simulates the protective and nurturing environment of a kangaroo pouch. It offers physiological and psychological benefits for both infants (preterm or full term) and parents by:
– Stabilizing the baby’s heart and respiratory rate
– Boosting brain, cognitive and motor development
– Improving baby’s sleep
– Enhancing breastfeeding
– Improving the bond with the baby
Maximize daily skin-to-skin time with your baby for his healthy development.
i. Benefits
For Babies promotes:
- Immune system
For Babies reduces:
- Gastric problems (colic, reflux, etc.)
- Respiratory and infection problems
- Bacterial meningitis
- Retinopathy of prematurity
- Sudden Infant Death Syndrome – SIDS
- Hospitalization
For Mothers promotes
- Faster weight loss after birth
- Immunity to infection
- Breast milk is always clean and at the right temperature
- Money saving
For Mothers reduces:
- Postpartum bleeding
- Risk of postpartum depression
- Breast and ovarian cancer
- Rheumatoid arthritis
- Lupus
- Osteoporosis (with age)
- Diabetes
- Cardiovascular disease

Did you know that Kangaroo Care not only offers benefits to infants but also boosts breastfeeding?
Kangaroo Care, also known as skin-to-skin contact releases hormones that improve breastfeeding and increase breast milk production!

In most cases, mothers can continue breastfeeding even when they’re sick. The antibodies produced by the mother to fight diseases will be passed on to the baby, building their own defenses!
Contact your physician to determine if you can breastfeed, however use a breastpump to stimulate continuous milk production.
For more information, contact us on 71 998822
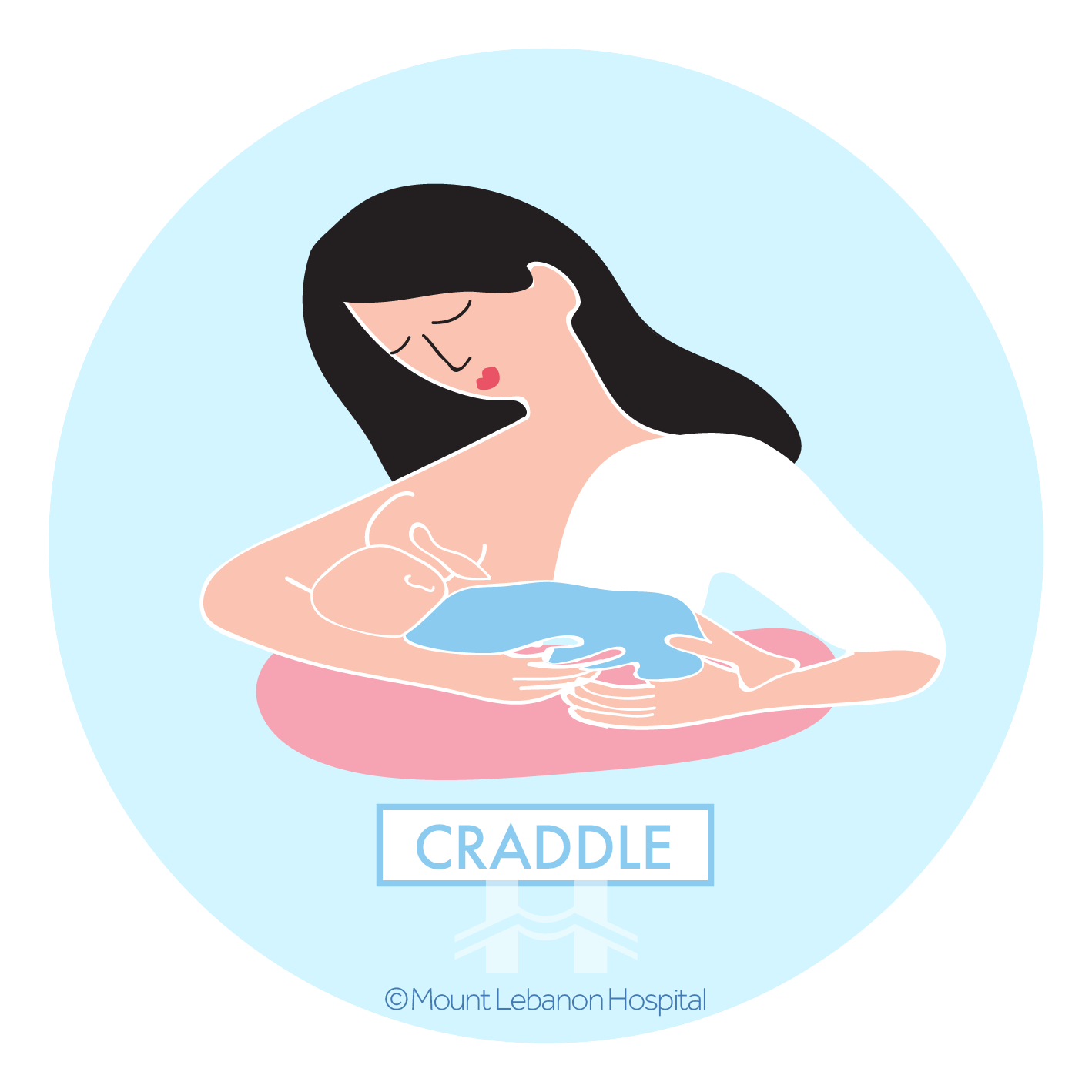
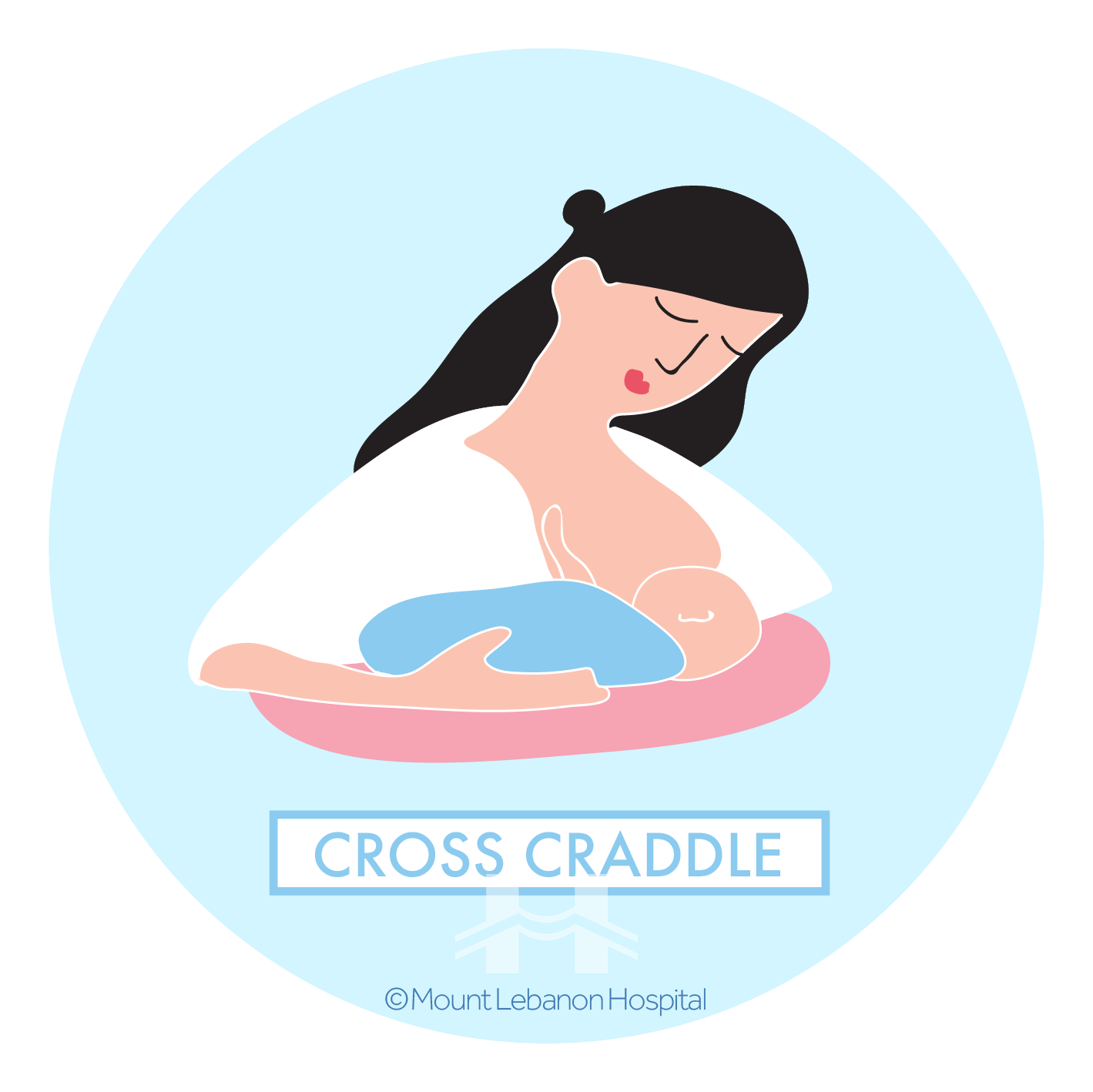
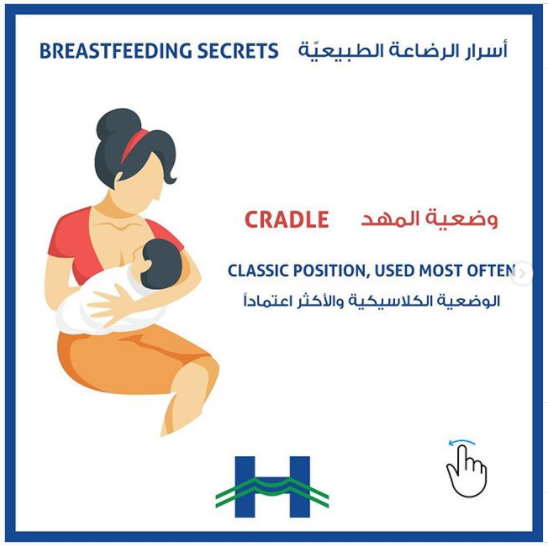
ii. Positions
Breastfeeding positions allow you to rest and choose the most adequate to suit your condition and needs.
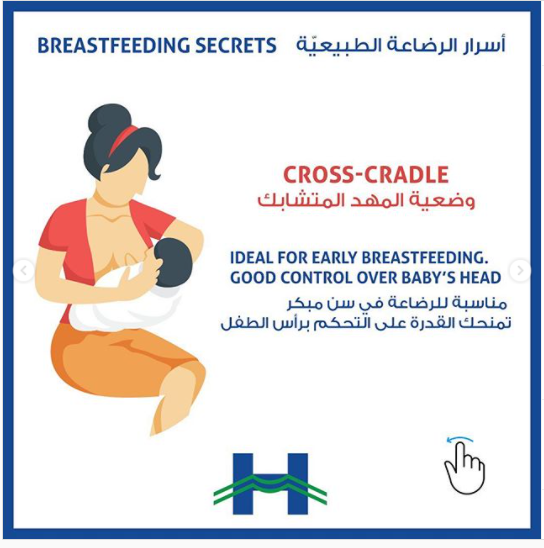
Cradle Hold & Cross Cradle Hold Position
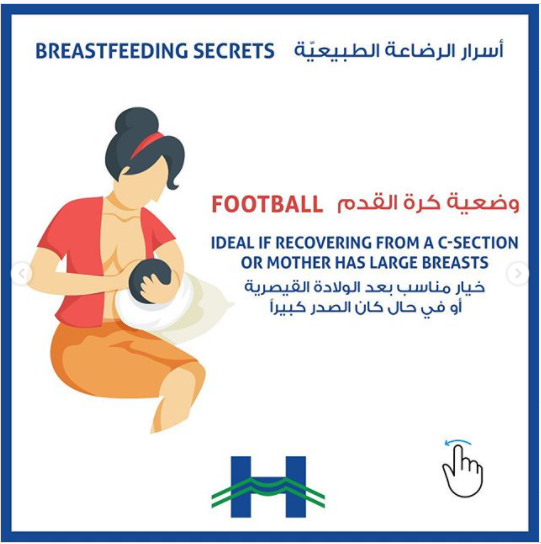
Football Hold Position

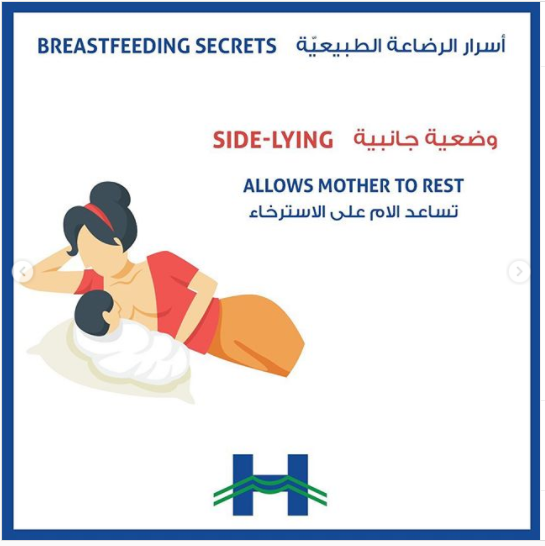
Side-Lying Position
iii. Baby’s hunger cues
- Fingers in their mouth
- Sucking on fingers
- Squirming
- Moving arms or legs
- Licking or smacking lips
- Opening and closing mouth
- Turning head side-to-side
- Balling up fists and holding them to chest
- Rooting when touched on the chin or cheek
- Crying

iv. Baby’s satiety signs
- Open, relaxed hands
- Relaxed, soft body
- Arms lie across lower body
- Falls asleep at the breast
- Turns head away
- Has “wet burps,” where milk dribbles out of the side of mouth
- Decreases or stop sucking on nipple
- Spits out the nipple on a bottle
v. How to help the baby burp
When burping your baby, repeated gentle patting on the back should do the trick.
1.Upright against chest.

2.Hold your baby sitting up, in your lap or across your knee.
Support your baby’s chest and head with one hand by cradling your baby’s chin in the palm of your hand.

3.Lay your baby on your lap on his or her belly.
Support your baby’s head and make sure it’s higher than his or her chest. Gently pat your baby’s back.

vi. Breast and nipple care
- Practice good hygiene:
- Wash hands before touching breasts;
- Keep breasts and nipples clean by washing them daily with warm water in the shower or bath;
- Avoid using soap on breasts since it can cause dry, cracked, and irritated skin.
- Wear a supportive bra: Choose a nursing bra or a regular bra that fits well, but not too tight. Cotton is an excellent choice since it allows the skin to breathe;
- Make sure baby is latching on correctly;
- Change breast pads often or until they are wet;
- Moisturize nipples with breast milk, let them air dry;
- Detach baby from breast correctly: Place finger in the corner of the mouth to break the suction between the mouth and breast;
- Treat breast engorgement: If your breasts become painfully congested, hard, and swollen, you can use cold cabbage leaves or cold compresses to reduce inflammation and relieve pain.
vii. Breast pump
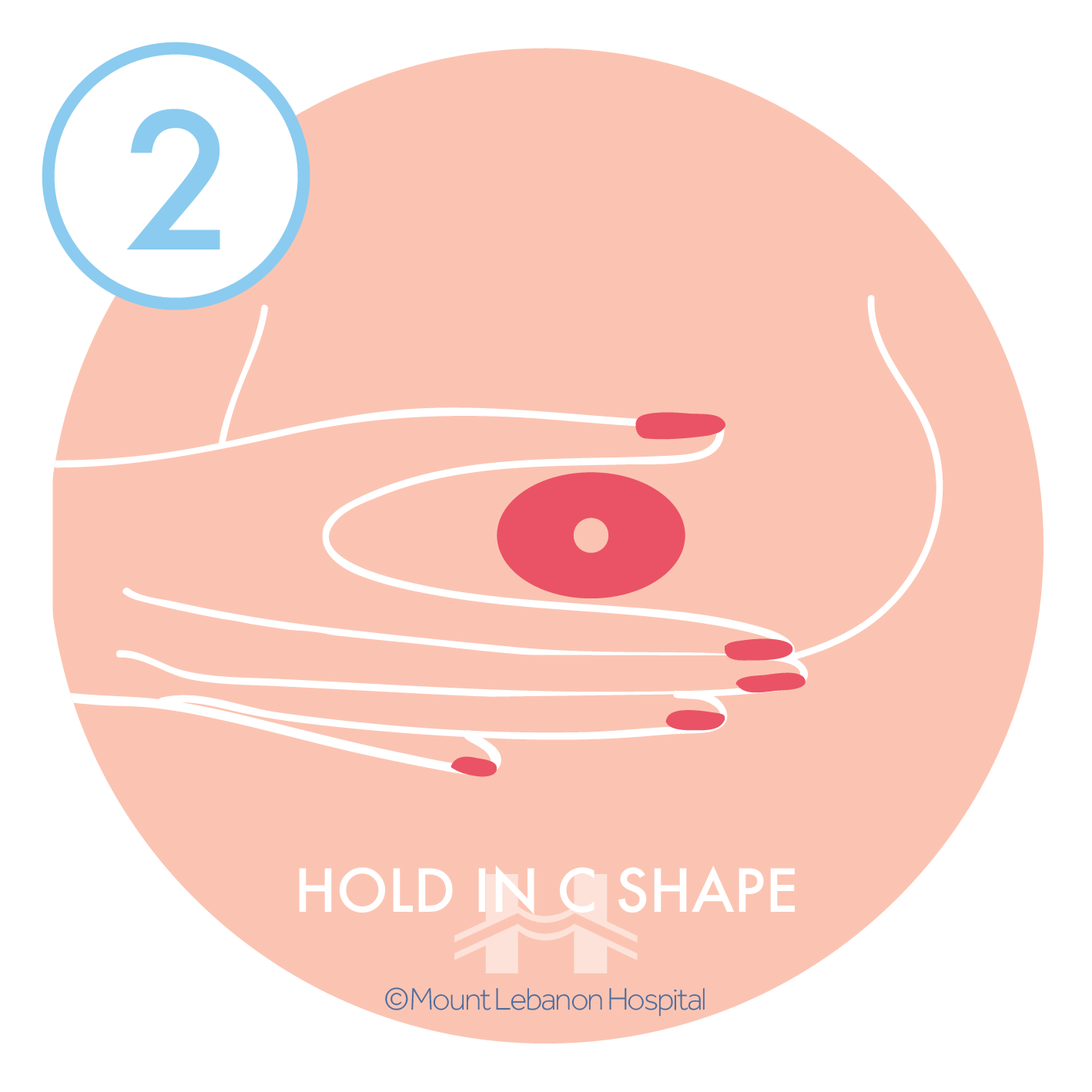
Breast milk can be pumped in several ways. Always keep in mind that before any steps, the following should be done:
1- Wash hands thoroughly
2- Apply hot water or a damp towel on breasts (or during the shower)
3- Massage breasts with your fingertips to eliminate any engorgement
Please Note: You can apply an ice pack, 10 mins before or after pumping, for breast pain.



![]()
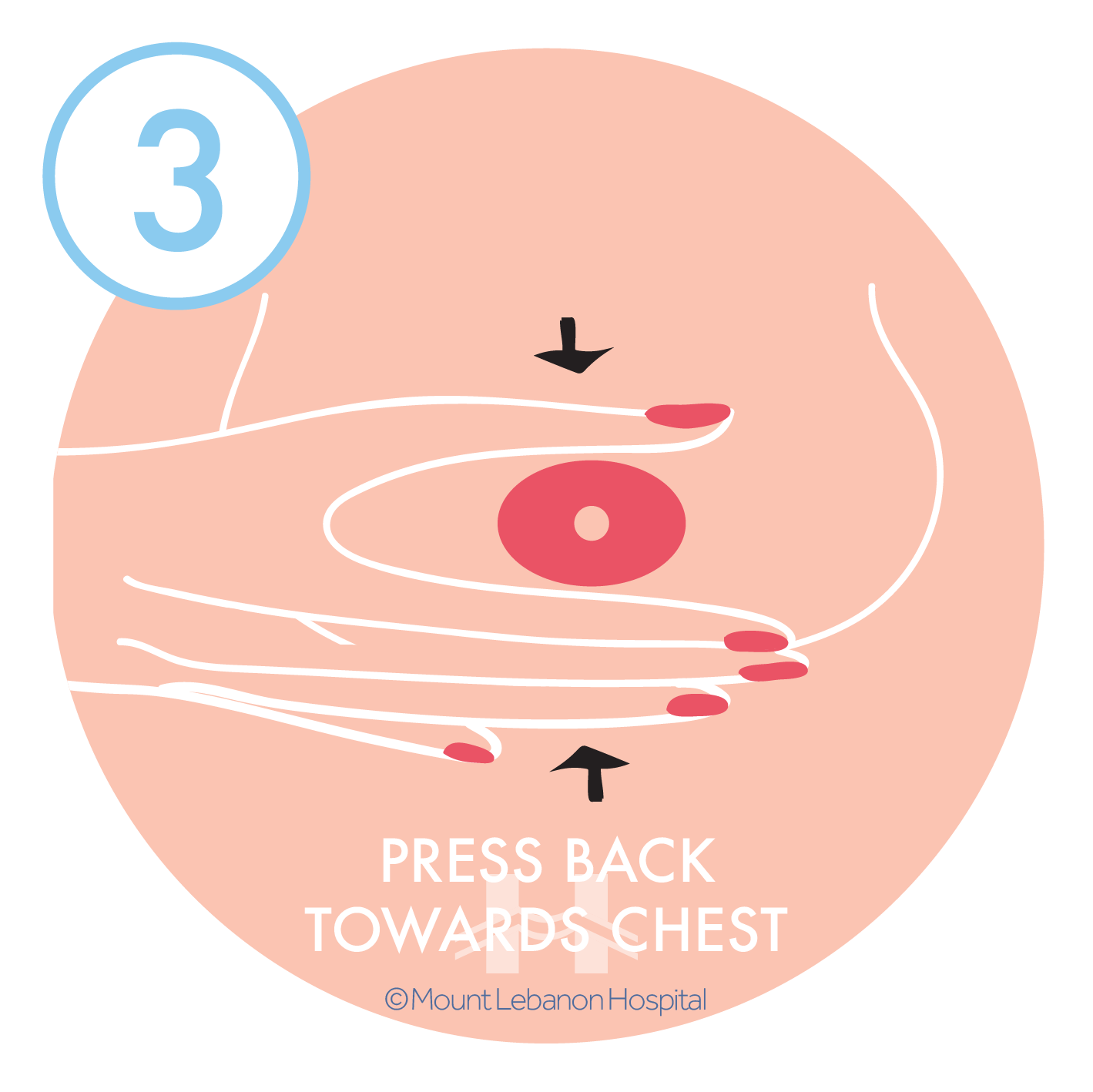
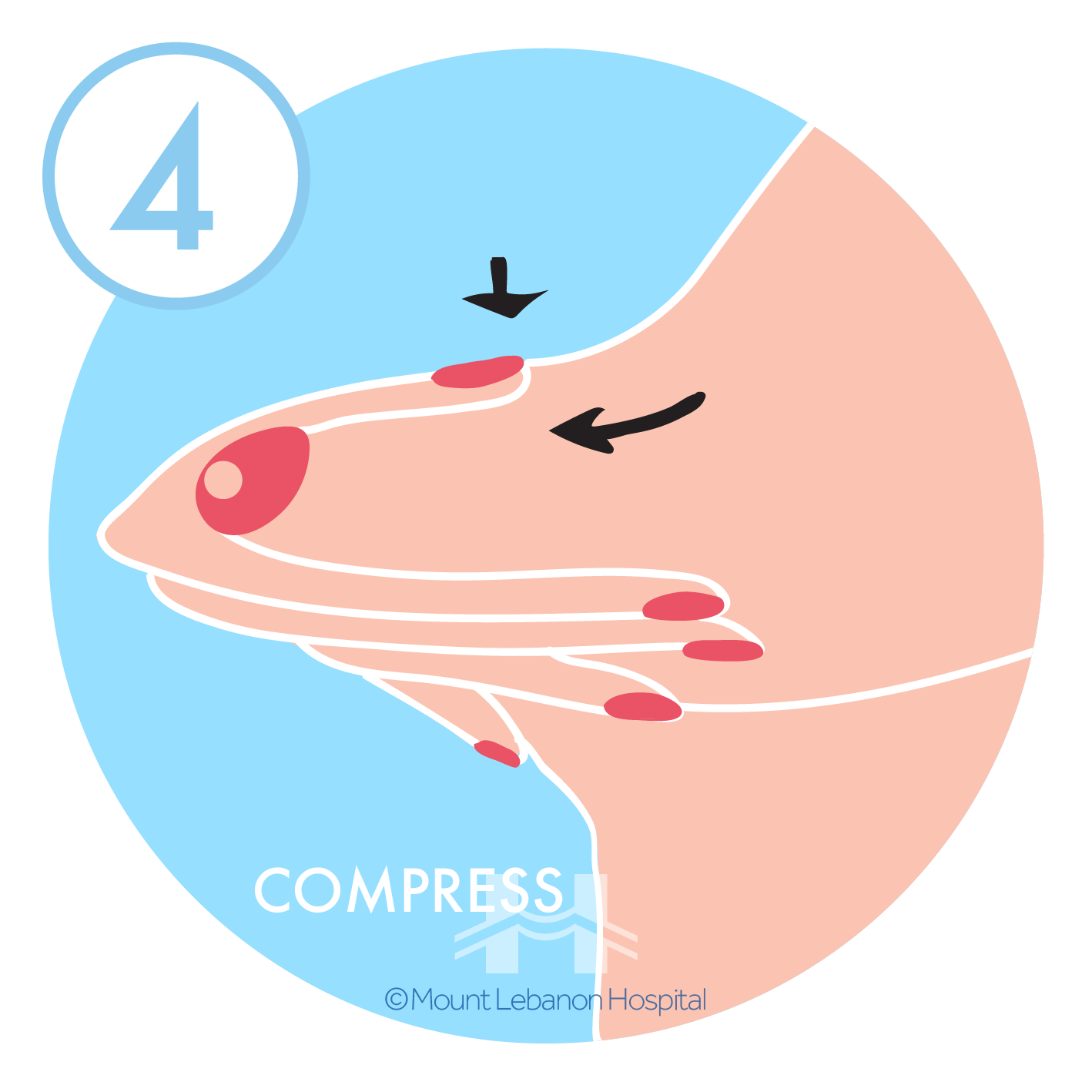
By hand:

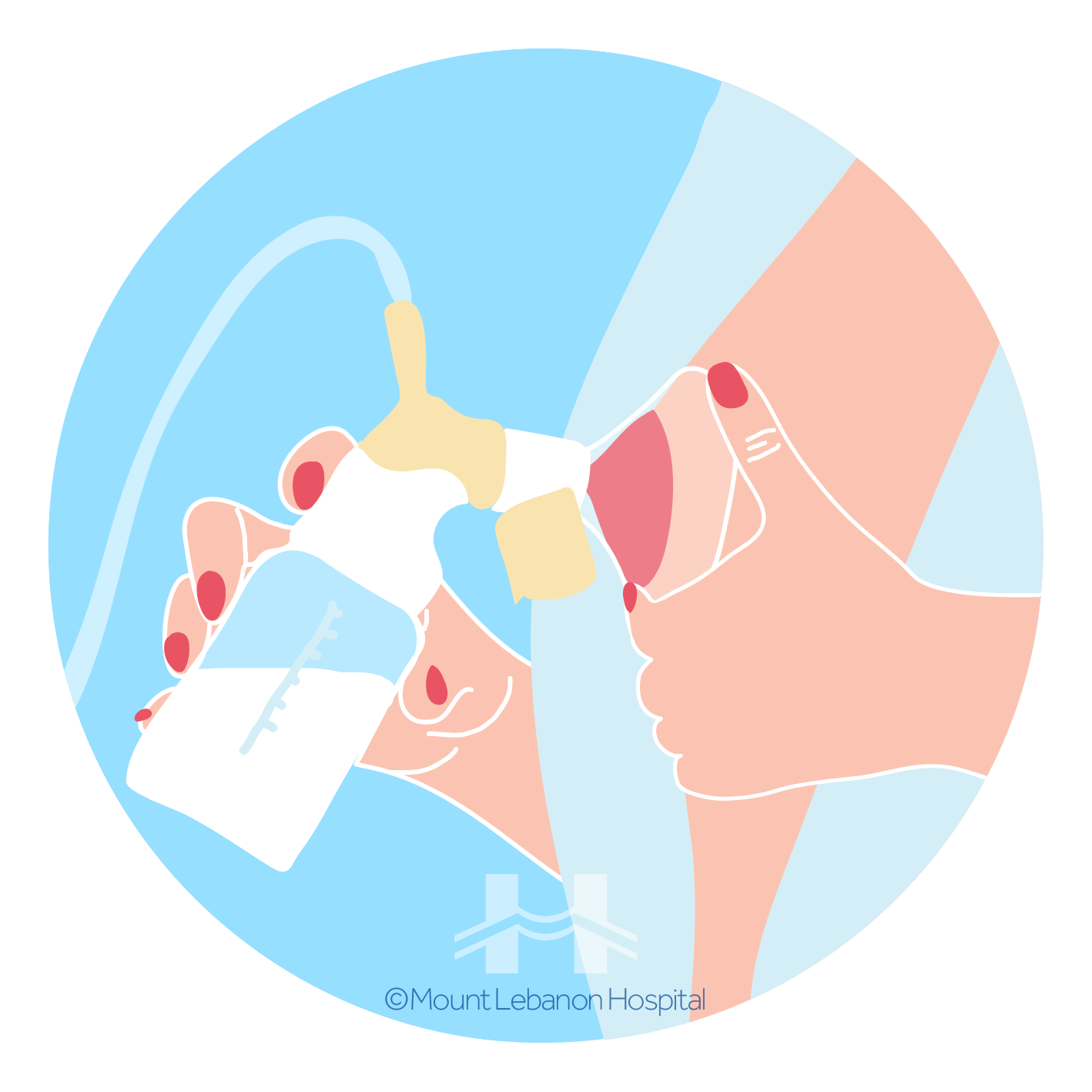
By a pump, always inspect the kit and tubing to make sure it is clean
Manual or electric:
viii. Milk storage
- Use breast milk storage bags, clean glass or plastic food containers with tight fitting lids;
- Use BPA free bottles;
- Clearly label the breast milk with the date it was expressed;
- Do not store breast milk in the refrigerator or freezer door, to protect breast milk from temperature changes;
- Freeze freshly expressed breast milk, right away to avoid wasting;
- When freezing breast milk, leave about an inch of space at the top of the container because breast milk expands as it freezes;
- Breast milk can be stored in an insulated cooler bag with frozen ice packs for up to 24 hours while traveling. Once you arrive at your destination, milk should be used right away, stored in the refrigerator, or frozen;
- Breast milk does not necessarily need to be warmed: if frozen, hold or let bottle sit under warm water;
- Never put breast milk bottle or bag in the microwave;
- Do not re-freeze.
|
Place |
Temperature |
Duration |
Important information |
|
Room temperature |
19°C to 25°C |
Up to 3 – 4 hours |
Containers must be covered and kept as cool as possible |
|
Smaller cooler with blue-ice pack |
-15°C to 4°C |
Only for transport |
Keep ice packs in contact with milk containers at all times, limit opening cooler bag. |
|
Refrigerator |
4°C |
48 hours |
Avoid spilling. Store in the back of the refrigerator’s main compartment. |
|
Refrigerator’s Freezer compartment with separate door |
-18°C |
4 months |
Store milk in the back of the freezer where the temperature is most constant. |
|
Deep in the freezer |
-20°C |
6 – 12 months |
ix. Sterilizing techniques
It is important to sterilize baby bottles before each use, for at least the first 12 months of baby’s life.
Sterilizing is the process of killing any harmful germs that may be clinging to surfaces of bottles and other equipment.
Clean used bottled thoroughly as soon as possible after feeding.
Put the lid and teat onto the bottle, and store them in a clean container in the fridge for 24 hours sterilizing, if you are not using them straight away.
There are a few different ways to sterilize:
Boiling:
- Fill saucepan with water
- Place utensils while removing air bubbles
- Bring water to boil for 5 minutes
- Turn off the stove
- Allow the water to cool down

Chemicals:
- Place the feeding equipment in the sterilizing solution, make sure it is completely under water and there are no air bubbles
- Leave the equipment in the sterilizing solution about 30 minutes, until needed
- Drain bottles, teats and lids before use
- Do not rinse off the sterilizing solution, as this exposes equipment to germs again
- Throw away the solution after 24 hours

Electric sterilizers:
- Make sure bottles and teats are placed with openings facing down in the sterilizer
- Keep bottles sterilized for up to 6 hours in the sterilizer with lid closed
- Follow instructions for adding water to the unit and turning it on
x. Pacifier
The use of pacifiers for breastfed babies is controversial. The decision to use a pacifier is up to the parents.
Pros:
- May gain more weight for Premature Babies
- Reduce the risk of sudden infant Death Syndrome – SIDS
- Can satisfy the desire for non-nutritive sucking
- Help to soothe a baby with reflux or colic
- Comfortable to baby during stressful or painful situations
- Helpful during travel on an airplane, can relieve painful pressure in the middle ear
Cons:
- The long-term use can cause problems with child’s teeth
- Children can become very attached to their pacifier
- Increase risk of ear infections
- Could get in the way of baby’s ability to latch on
- Cause breast problems such as sore nipples, engorgement, plugged milk ducts, and mastitis. And can interfere with the development of milk supply
- May lead to early weaning
- Tire out a sleepy baby making breastfeeding more difficult
- Younger babies who use pacifiers tend to cry when the pacifier falls out of their mouths
- The overuse of a pacifier during the day could prevent your baby from getting enough milk and wake up more often during the night to eat
Recommendations:
- Delay pacifier use (4 to 8 weeks) for healthy babies
- Choose the silicone one-piece
- Keep it clean (wash and sterilize)
- Never hang a pacifier around the baby’s neck
- Do not use the nipple from a bottle as a pacifier, baby might choke
- Keep it safe: Specify the size of the pacifier for the baby’s age and replace pacifiers often
- Do not sugarcoat it
C. Baby care
i. Bathing
Every bath time can be a special bonding time with the newborn.
Preparation:
- Heat the room beforehand, at least 24°C
- Pick a warm room with a flat surface changing table
- Cover the surface with a thick towel
- Sponge baths are perfect for the first few weeks
- Use baby specific products
- Clean washcloth, bath towel, diaper, clothes
- Plain cotton cleaning pads for the baby’s face
- Check water temperature, warm water (38°C) and baby’s body temperature (36.5 to 37°C)
- Avoid feeding a newborn at least 1 to 2 hours before bath time
- Do not bathe the baby, if he’s hungry or he’s got a fever (38°C)
Bathing basics:
- Bathe a baby every day;
- Place all bath supplies within hand reach to ensure easy access while one hand is always supporting the baby
- Fill the tub with few inches of warm water (36°C). Check the temperature with the inner side of the wrist (a thermometer would help)
- Support baby’s head and neck, gently place him/her in the tub. Support the head and neck with one arm at all times
- Start, with a washcloth behind the ears, then move to the neck, elbows, knees, between fingers and toes
- Gently clean the rest of the body, bottom and genitals
- Wash diaper area from front to back in the end
- Do not pull the foreskin back in case baby boy is uncircumcised
- Wash baby girls from front to back
- All babies enjoy being in water. Keep pouring water over their body to ensure that they stay warm
- Wash baby hair after washing the body, to avoid colds
- Tilt the head back
- When done. remove baby gently from the tub while supporting head and neck and quickly wrap in a towel
- Gently wipe until dry, and keep wrapped in a towel
- Use a baby moisturizer, because the baby’s skin is delicate and tends to dry
- Use cotton pads to clean baby’s eyes. Dip them in warm water and gently wipe outwards
- Use one pad for each eye. Use cotton pads to clean the baby’s mouth, nose, face, neck and ears
Precautions:
- Do not leave the baby unattended in the water even for a second
- Do not keep the water running while the baby is in the tub. Water temperature changes can be sudden and unexpected
- Do not use large quantities of soap. This can dry the baby’s skin and cause rashes
- Bath duration should not exceed 5 minutes. Excessive time in a bath can exhaust the baby
Some Tips:
- Before scheduling bath time, keep in mind that babies will most likely fall asleep after a warm bath
- Clean only what you can see, do not try to clean the ear canal or inside the nose
- Place a non-slipping mat under the bathtub and bathing area, to prevent unexpected accidents such as slipping
- After shower, put a nappy on your baby to avoid urinating accidents
- Stretch the neck of a singlet and put it on from the back. Be careful it doesn’t touch your baby’s face as you pull the front over the head
- Gently place baby’s arms through the sleeves
- If you’re dressing the baby in a jumpsuit, unbutton or unzip it and lay him/her on top. Place his/her arms and legs into the sleeves and do up the zip or snap fasteners
- Do not hold extremities such as fingers and toes, but rather wrists and ankles
ii. Umbilical cord care
After birth the umbilical cord is clamped and cut, leaving a stump behind, it changes in color from yellowish-green to brown to black before falling off in about 7 – 15 days.
In order to prevent infection, it is important to keep the stump clean, nevertheless, water does not increase the rate of infection or take longer to fall off.
After the fall of the umbilical cord, it takes about 10 days for the area to heal completely. Continue disinfectant care for about one week to avoid infection.
iii. Diaper change
It’s important to make sure you have everything you need (or could need) before you begin, such as the following:
- A safe, clean place: a changing table or mat, with safety straps.
- Diapers: In the correct size.
- Something to wipe the baby with:
- Warm water and a cloth during the first weeks of life (recommended by pediatricians)
- Non Alcoholic baby wipes
- Nappy cream or ointment (if needed)
Changing a Diaper Step by Step:
- Wash your hands and make sure supplies are nearby
- Lay your baby on the back
- Unfasten the diaper tabs
- Raise child’s bottom off the diaper by gently lifting ankles with one hand
- Slide the diaper away from the baby and place it nearby, out of reach with the other hand
- Wipe the baby clean to avoid rashes. Always go from front to back to prevent any infection
- Slide a clean diaper under baby’s bottom, making sure the strips are under your child’s bottom
- Before closing the diaper, apply any rash ointment or cream (if needed)
- Close the new diaper
- If you are not using specially cut newborn diapers, be sure to fold the diaper down to avoid umbilical stump irritation until it falls off
iv. Skin care

Cotton buds are non-biodegradable; its extensive use is harmful for the environment.
We all know our ears cleanse their own earwax; why do we still use cotton buds? A swipe with a cotton cloth after shower cleans the ear’s outer area without harming the canal and eardrum.
Baby’s skin is very sensitive, always check with the pediatrician about any product that you will be using and avoid products with paraben, formaldehydes, or fragrances.
- Cleanser (body wash): Soap-free liquids are a good choice
- Shampoo: Tearless is best
- Nappy cream: Use petroleum jelly or zinc oxide cream
- Wipes: Alcohol-free or water and a washcloth
- Moisturizer: choose creams or ointments over lotions (petroleum gel)
- Laundry detergents: Liquid detergents rinse out better than flaked ones
v. Nail trimming
The best time is while baby is sleeping. Another good time is right after a bath, when your baby’s nails are softest.
- Make sure you have enough light to see what you’re doing
- Use a pair of baby scissors or clippers made especially to use on tiny fingers
- Press the finger pad away from the nail to avoid nicking the skin
- Keep a firm hold on baby’s hand as you clip
- Cut fingernails along the curve of the finger
- Cut toenails straight across. Then use an emery board to smooth out rough edges
Doctors recommend using only an emery board in the first few weeks of a baby’s life because nails are very soft. And new parents are also more likely to accidentally clip their baby’s skin.
vi. Sleeping
Sleep is especially important for children as it promotes mental and physical development. In fact, the growth hormone (GH) is primarily secreted during deep sleep

To ensure their healthy development, babies should sleep:
1- On their backs
2- With their head uncovered
3- On a firm mattress
4- In their parents’ room for 6 months
5- In tempered areas (not too hot)
For a safe sleep:
- Always place your baby on the back, to reduce the risk of Sudden infant death syndrome – SIDS
- Use a firm sleep surface, covered by a fitted sheet
- Newborns should not sleep in an adult bed, on a couch, or on a chair unattended
- Keep soft objects, toys and loose bedding out of the baby’s sleeping area
- Pacifier during naptime should be detached from the string
- Check room temperature regularly, it should not be too hot or too cold
- Keep rooms at a normal temperature, about 22.2°C to 24° C
- The baby should be dressed just like the parents and others in the room
vii. Fever
A newborn’s temperature regulation system is immature. Fever among babies can be caused by many reasons. Call the pediatrician immediately if the baby is younger than 3 months old and has a rectal temperature of 38°C or higher.
Overheating
While it is important to keep a baby from becoming chilled, a baby can also become overheated with many layers of clothing and blankets. This can occur at home, near heaters or heat vents. It can also occur when a baby is over bundled in a heated car.
- Avoid placing a baby in direct sunlight, even through a window
- Never leave a baby unattended in a hot car even for a minute
- An overheated baby may have a hot, red, or flushed face, and may be restless. To prevent overheating
Low fluid intake or dehydration
Some babies may not take in enough fluids which causes a rise in body temperature. This may happen around the second or third day after birth. If breast milk or formulas are not replaced with increased feedings, dehydration can develop and cause serious complications.
viii. Visitors
It is recommended:
1- Wash their hands and use sanitizer before holding or touching the baby
2- No kissing
3- No flash in photographs
4- Do not approach the baby if they are sick
ix. Leaving the house for the first time
Make a checklist of a bag that should be with you at all times. It should include:
- 3 underwear
- 3 pajamas
- 1 baby cap
- 4 cotton cloths
- 1 blanket
- 2 soothers
- 4 servings of milk formula (if you are breastfeeding this would not be a problem)
- 4 baby bottles
- 1 bottle of water
- Sterilizing solution
- Changing matt
- Wipes
- 6 to 8 diapers
- Nappy cream
Insure your baby’s security during travels with a car seat.
- Always use a car seat, never put the baby in your lap;
- Practice installing the car seat in and out of the car without the baby in it;
- Car seat should not be placed on the front passenger seat;
- Verify car seat’s stability;
- Never leave your baby unattended in the car;
- Make sure the car seat is buckled securely in the car;
- All car seats have an expiration date (usually 6 years).
x. Contact your pediatrician immediately if the baby has
- A rectal temperature of 38°C;
- Blood in vomit or stool;
- Difficulty breathing;
- Signs of dehydration;
- Yellow skin or eyes;
- A seizure;
- Any type of poisoning;
- Unstoppable bleeding;
- Sleeps More than usual;
- Is not able to move.
D. Sex
You can resume sexual activity when:
- You have recovered (either from normal vaginal delivery or C-section delivery);
- Your bleeding has stopped;
- You and your partner feel comfortable.
E. Postpartum rehabilitation
- Vaginal discharge (Lochia):
After vaginal delivery, Lochia is a vaginal discharge, with a stale musty odor like menstrual discharge, dark red color for the first three days after delivery. A few small blood clots are normal.
- Urination contractions:
Discomfort is common while urinating, but contact your physician if you feel pain or difficulty while urinating.
- Incontinence:
During delivery your muscles stretched, and may cause temporary loss of urinary or bowel control. This may happen when you laugh, cough or strain.
- Constipation:
After delivery, the first bowel movement might be delayed to the 3rd or 4th day. to avoid discomfort, drink at least 10 to 12 glasses of water and include fruits and vegetables to your diet. Your physician may prescribe an over-the-counter stool softener.
- Menstruation:
If you are breastfeeding, you may not get your period until your baby stops breastfeeding. Be aware, you might get pregnant while breastfeeding, even if you are not getting your period. If you are bottle feeding, you will get your period 6 to 12 weeks after delivery. Always remember that the first few periods will be irregular.
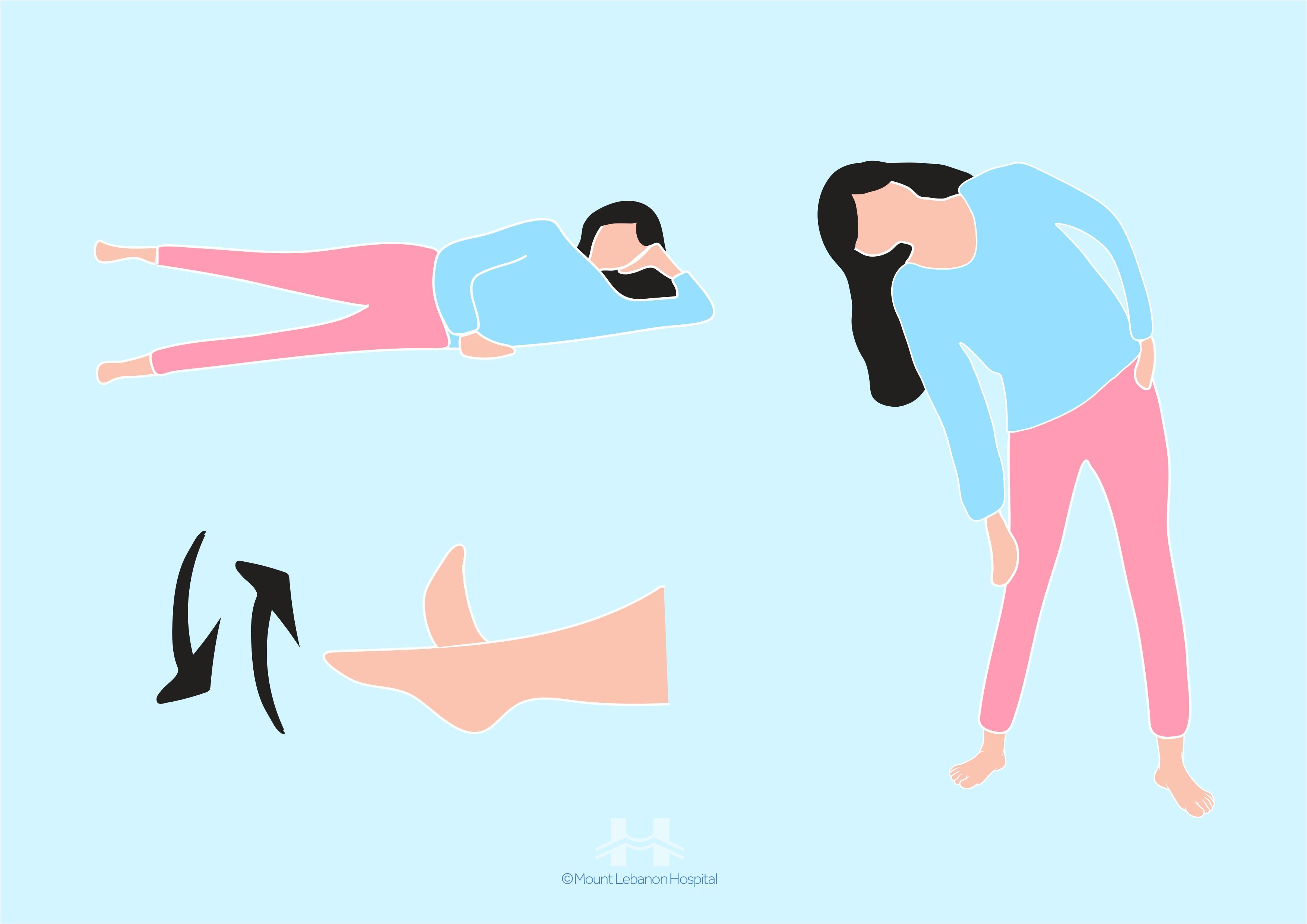
Exercises after Delivery:
If you are aiming to lose weight and return to your “pre-pregnancy” weight, follow a consistent and healthy diet. Plan a varied and easy to follow routine:
- Choose a fun activity, because exercising after giving birth should be enjoyable without punishing too hard;
- Adopt a healthy lifestyle;
- Schedule regular and varied exercises into daily activities;
- It is recommended to start strengthening pelvic floor muscles before exercising abdominal muscles;
- In the first 6 to 8 weeks after C-section delivery, mother should not lift weights heavier than baby’s weight;
- Consult a physician or physical therapist for a postpartum care plan.

Stop exercising and contact a physician if you have:
- Severe or chronic pain;
- Increased vaginal bleeding;
- Faintness;
- Nausea;
- Shortness of breath;
- Extreme fatigue and muscle weakness.
Thank you for choosing Mount Lebanon Hospital to be part of this new phase of your life. Our highly trained OBGYNs, Midwives, Physiotherapists and Psychotherapists are always available for your help. We can’t wait to witness your family growing. If you have any questions or concerns Mount Lebanon Hospital’s Obstetrics and Gynecology department is always ready to assist you. We also offer Home Care Services in order to take care of the mother and baby.
Mount Lebanon Hospital
Committed to Excellence in Healthcare
Mikhael Gharios street, Beirut, Lebanon
www.mlh.com.lb – mlh@mlh.com.lb – +961 5 957 000 – 15271